Articles and Other Useful Information
10 REASONS WHY YOU SHOULD TAKE CARE OF YOUR PETS TEETH.
THE IMPORTANCE OF DENTAL RADIOGRAPHS
FEBRUARY IS NATIONAL PET DENTAL HEALTH MONTH.
WHATS A FECAL TEST FOR ANYWAYS?
KEY FACTS ABOUT CANINE INFLUENZA (DOG FLU)
5 TIPS FOR SURVIVING YOUR DOGS CANCER TREATMENT
SKIN DISEASE DUE TO FOOD ALLERGIES IN CATS.
IS A REPTILE THE RIGHT PET FOR YOU?
HAVE YOU CHECKED YOUR PETS CHIP?
IT IS NATIONAL IMMUNIZATION AWARENESS MONTH. ARE YOUR PET’S VACCINATIONS UP-TO-DATE?
HOW TO MANAGE MULTIPLE PETS UNDER ONE ROOF.
IS YOUR CAT NOT MAKING IT INTO THE BOX?
HOW YOUR DOG’S BEHAVIOR CAN CHANGE WITH AGE.
SEPARATION ANXIETY IN DOGS AND WHAT YOU SHOULD DO
REDUCING YOUR DOGS FEAR OF THE VETERINARIAN.
HOME OWNERS INSURANCE AND WHAT YOU SHOULD KNOW WHEN HAVING PETS.
WARM WEATHER CONCERNS FOR RABBITS
PREVENTING DOG BITES BY LEARNING TO GREET DOGS PROPERLY
6 TIPS FOR SOOTHING YOUR DOG’S FEAR OF THUNDER
ENRICHMENT – 8 EASY WAYS TO INCREASE YOUR DOG’S QUALITY OF LIFE
LIVING WITH AN ARTHRITIC SENIOR CAT
BEHAVIOR PROBLEMS IN SENIOR PETS
NUTRITIONAL MANAGEMENT OF GASTROINTESTINAL DISEASE
STRUCTURE AND FUNCTION OF THE GASTROINTESTINAL TRACT IN CATS
DOGGIE PLAY DATES: ARE THEY FOR YOUR DOG?
KEYS TO KEEPING A BIRD HEALTHY
10-REASONS-WHY-YOU-SHOULD-TAKE-CARE-YOUR-PETS-TEETH
FEBRUARY-IS-NATIONAL-PET-DENTAL-HEALTH-MONTH.ASPX
FEMALE DOGS ARE MORE LIKELY TO DEVELOP THIS CONDITION.
STRAINING TO URINATE IS THE FIRST SIGN OF THIS SERIOUS CONDITION.
THE DOGS HAVE THE POWER. FLOWER POWER, THAT IS.
HAIR LOSS IN YOUR PET COULD BE A SIGN OF THIS DISEASE.
THIS SEVERE LIVER CONDITION CAN OCCUR IF YOUR CAT STOPS EATING.
SHY DOG? FOLLOW THESE STEPS TO HELP BOOST HIS OR HER CONFIDENCE.
PETS CAN FEEL STRESS DURING THE HOLIDAYS, TOO. ALLEVIATE SOME OF THAT STRESS WITH THESE TIPS.
MOST PET OWNERS MAY NOT BE AWARE THAT MISTLETOE IS POISONOUS TO DOGS. LEARN ABOUT OTHER PET POISONS.
AS YOU DECORATE FOR THE HOLIDAYS, BE AWARE OF THE HEALTH HAZARDS TINSEL AND OTHER FESTIVE FRILLS POSE FOR PETS.
THANKSGIVING IS JUST AROUND THE CORNER. WITH THIS RECIPE, YOUR PUP CAN ENJOY A HOLIDAY DINNER, TOO.
THIS CAT LOVER HAS CREATED AN INNOVATIVE WAY FOR HIS CAT TO BOTH EXPLORE AND EAT!
APPROXIMATELY 2% TO 3% OF ALL CATS ARE INFECTED WITH THIS VIRUS, WHICH IS THE LEADING CAUSE OF CANCER IN CATS.
SMALL PURPLE SPOTS ON YOUR DOG’S SKIN MAY BE A SIGN OF THIS CANCER.
AS CATS GET OLDER, THEIR NORMAL, FAMILIAR BEHAVIORS MAY START TO CHANGE. KNOW WHAT TO EXPECT.
A WAGGING TAIL DOES NOT ALWAYS MEAN A DOG IS HAPPY. DISCOVER WHAT THAT WAGGING COULD MEAN AND 4 OTHER COMMON BEHAVIOR MYTHS.
SOME NATURAL BEHAVIORS OF CATS CAN BE DESTRUCTIVE TO THE HOME, BUT SOMETHING CAN BE DONE.
IT IS NATIONAL PET DIABETES MONTH, NOVEMBER. RECOGNIZE THE SIGNS OF DIABETES IN YOUR PET AND TEST YOUR KNOWLEDGE.
RADIOLOGY IS MORE THAN ULTRASONOGRAPHY AND CT SCANNING. NUCLEAR MEDICINE IS CONSIDERED RADIOLOGY, TOO.
GOLDEN RETRIEVERS HAVE A HIGHER RISK OF DEVELOPING THIS CANCEROUS CONDITION.
PREPARING FOR YOUR PET’S CANCER CONSULTATION MAY SEEM OVERWHELMING. HERE ARE SOME TIPS ON PREPARING FOR THE VISIT.
MANY PET OWNERS WORRY ABOUT PUTTING THEIR PET UNDER ANESTHESIA. KNOWING MORE ABOUT ANESTHESIA MAY HELP REDUCE CONCERN.
DID YOU KNOW THAT SPAYING OR NEUTERING YOUR PET CONTRIBUTES TO WELLNESS, TOO?
HEARTWORM TESTING AND PREVENTION ARE ESSENTIAL TO A PET’S WELLNESS. KNOW HOW HEARTWORM DISEASE CAN AFFECT YOUR DOG.
KNOW WHAT TO DO WHEN YOUR PET HAS A POISON EMERGENCY.
TIMING IS EVERYTHING. CREATING A REGULAR FEEDING SCHEDULE IS JUST ONE WAY TO HELP MANAGE YOUR DIABETIC DOG’S DIET.
DIABETES MELLITUS – INSULIN TREATMENT IN DOGS
THIS HANDOUT PROVIDES DETAILED INFORMATION ON INSULIN ADMINISTRATION. FOR MORE INFORMATION ABOUT DIABETES MELLITUS, SEE THE FACT SHEETS “DIABETES MELLITUS – GENERAL INFORMATION”, AND “DIABETES MELLITUS – PRINCIPLES OF TREATMENT”.
WHAT IS DIABETES MELLITUS?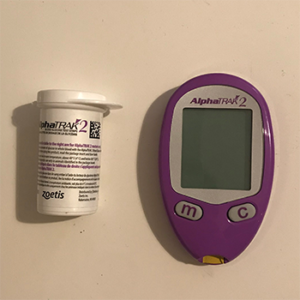 DIABETES MELLITUS IN DOGS IS CAUSED BY THE FAILURE OF THE PANCREAS TO REGULATE BLOOD SUGAR. IN THE DOG, DIABETES MELLITUS IS USUALLY INSULIN DEPENDENT DIABETES MELLITUS (ALSO CALLED TYPE 1 DIABETES). THIS TYPE OF DIABETES USUALLY RESULTS FROM DESTRUCTION OF MOST OR ALL OF THE BETA-CELLS THAT PRODUCE INSULIN IN THE PANCREAS. AS THE NAME IMPLIES, DOGS WITH THIS TYPE OF DIABETES REQUIRE INSULIN INJECTIONS TO STABILIZE BLOOD SUGAR LEVELS.
DIABETES MELLITUS IN DOGS IS CAUSED BY THE FAILURE OF THE PANCREAS TO REGULATE BLOOD SUGAR. IN THE DOG, DIABETES MELLITUS IS USUALLY INSULIN DEPENDENT DIABETES MELLITUS (ALSO CALLED TYPE 1 DIABETES). THIS TYPE OF DIABETES USUALLY RESULTS FROM DESTRUCTION OF MOST OR ALL OF THE BETA-CELLS THAT PRODUCE INSULIN IN THE PANCREAS. AS THE NAME IMPLIES, DOGS WITH THIS TYPE OF DIABETES REQUIRE INSULIN INJECTIONS TO STABILIZE BLOOD SUGAR LEVELS.
WHAT DO I NEED TO KNOW ABOUT INSULIN TREATMENT FOR DIABETES MELLITUS?
“THE MAIN TREATMENT FOR REGULATING BLOOD GLUCOSE IS THE ADMINISTRATION OF INSULIN BY INJECTION.”
IN DIABETIC DOGS, THE MAIN TREATMENT FOR REGULATING BLOOD GLUCOSE IS THE ADMINISTRATION OF INSULIN BY INJECTION. DOGS WITH DIABETES MELLITUS REQUIRE ONE OR MORE DAILY INSULIN INJECTIONS, AND ALMOST ALL REQUIRE SOME SORT OF DIETARY CHANGE. ALTHOUGH THE DOG CAN GO A DAY OR SO WITHOUT INSULIN AND NOT HAVE A CRISIS, THIS SHOULD NOT BE A REGULAR OCCURRENCE; TREATMENT SHOULD BE LOOKED UPON AS PART OF THE DOG’S DAILY ROUTINE. THIS MEANS THAT YOU, AS THE DOG’S OWNER, MUST MAKE BOTH A FINANCIAL COMMITMENT AND A PERSONAL COMMITMENT TO TREAT YOUR DOG. IF ARE OUT OF TOWN OR GO ON VACATION, YOUR DOG MUST RECEIVE PROPER TREATMENT IN YOUR ABSENCE.
WE’RE HERE TO HELP! VISIT VCAPETDIABETES.COM TO WATCH A VIDEO ON HOW TO GIVE AN INSULIN INJECTION, MONITOR BLOOD GLUCOSE WITH OUR EDIARY, FIND EXPERT ADVICE AND GET SUPPORT FROM OUR INTERACTIVE COMMUNITY TO HELP MANAGE YOUR DOG’S DIABETES.
INITIALLY, YOUR DOG MAY BE HOSPITALIZED FOR A FEW DAYS TO DEAL WITH ANY IMMEDIATE CRISIS AND TO BEGIN THE INSULIN REGULATION PROCESS. THE “IMMEDIATE CRISIS” IS ONLY GREAT IF YOUR DOG IS SO SICK THAT IT HAS QUIT EATING AND DRINKING FOR SEVERAL DAYS. DOGS IN THIS STATE, CALLED DIABETIC KETOACIDOSIS, MAY REQUIRE A SEVERAL DAYS OF INTENSIVE CARE. OTHERWISE, THE INITIAL HOSPITALIZATION MAY BE ONLY FOR A DAY OR TWO WHILE THE DOG’S INITIAL RESPONSE TO INSULIN INJECTIONS IS EVALUATED. AT THAT POINT, YOUR DOG RETURNS HOME, WHERE YOU WILL CONTINUE TO ADMINISTER MEDICATION. AT FIRST, RETURN VISITS ARE REQUIRED EVERY THREE TO SEVEN DAYS TO MONITOR PROGRESS. IT MAY TAKE A MONTH OR MORE TO ACHIEVE GOOD INSULIN REGULATION. YOUR VETERINARIAN WILL WORK WITH YOU TO TRY TO ACHIEVE CONSISTENT REGULATION, BUT SOME DOGS ARE DIFFICULT TO KEEP REGULATED.
 CONSISTENT TREATMENT IS A VITAL COMPONENT OF THE PROPER MANAGEMENT OF THE DIABETIC DOG. YOUR DOG NEEDS CONSISTENT ADMINISTRATION OF INSULIN, CONSISTENT FEEDING, AND A STABLE, STRESS-FREE LIFESTYLE. ALTHOUGH IT IS NOT ESSENTIAL, YOUR DOG SHOULD LIVE INDOORS TO MINIMIZE UNCONTROLLABLE VARIABLES THAT CAN DISRUPT REGULATION.
CONSISTENT TREATMENT IS A VITAL COMPONENT OF THE PROPER MANAGEMENT OF THE DIABETIC DOG. YOUR DOG NEEDS CONSISTENT ADMINISTRATION OF INSULIN, CONSISTENT FEEDING, AND A STABLE, STRESS-FREE LIFESTYLE. ALTHOUGH IT IS NOT ESSENTIAL, YOUR DOG SHOULD LIVE INDOORS TO MINIMIZE UNCONTROLLABLE VARIABLES THAT CAN DISRUPT REGULATION.
“YOU MAY BE PLEASANTLY SURPRISED AT HOW EASY IT IS AND HOW WELL YOUR DOG TOLERATES THE INJECTIONS.”
“MANY PEOPLE ARE INITIALLY FEARFUL OF INFLICTING PAIN OR HARM BY GIVING INSULIN INJECTIONS. HOWEVER, THIS FEAR IS UNFOUNDED, SINCE THE DISPOSABLE INJECTION NEEDLES ARE EXTREMELY SHARP AND CAUSE MINIMAL PAIN, THE INSULIN DOES NOT STING OR OTHERWISE HURT ON INJECTION, AND THE INJECTIONS ARE GIVEN UNDER THE SKIN IN AREAS WHERE IT IS IMPOSSIBLE TO DAMAGE INTERNAL STRUCTURES. ONCE YOU ARE SHOWN HOW TO GIVE THEM, YOU MAY BE PLEASANTLY SURPRISED AT HOW EASY IT IS AND HOW WELL YOUR DOG TOLERATES THE INJECTIONS.
HOW IS INSULIN STORED?
INSULIN IS A HORMONE THAT WILL LOSE ITS EFFECTIVENESS IF EXPOSED TO DIRECT SUNLIGHT OR HIGH TEMPERATURES. IT SHOULD BE KEPT IN THE REFRIGERATOR, BUT IT SHOULD NOT BE FROZEN. IF YOU HAVE ANY DOUBT ABOUT THE STORAGE OF YOUR PET’S INSULIN, IT IS SAFER TO REPLACE IT RATHER THAN RISK USING INEFFECTIVE INSULIN. INSULIN IS SAFE AS LONG AS IT IS USED AS DIRECTED, BUT IT SHOULD BE KEPT OUT OF THE REACH OF CHILDREN.
INSULIN COMES IN AN AIRTIGHT BOTTLE THAT IS LABELED WITH THE INSULIN TYPE AND THE CONCENTRATION. IT IS IMPORTANT TO MAKE SURE YOU MATCH THE INSULIN CONCENTRATION WITH THE PROPER INSULIN NEEDLES. INSULIN NEEDLES SHOW THEIR MEASUREMENT IN “UNITS PER ML”, WHICH MUST CORRESPOND TO THE CONCENTRATION OF THE INSULIN YOU ARE USING. THERE ARE TWO COMMON FORMS OF INSULIN AND CORRESPONDING SYRINGES: U-100 AND U-40. YOUR VETERINARIAN WILL INSTRUCT YOU ON WHICH TYPE OF INSULIN YOU ARE USING AND WHICH TYPE OF SYRINGE YOU SHOULD USE.
HOW SHOULD I DRAW UP THE INSULIN?
BEFORE ADMINISTERING THE INSULIN, YOU MUST MIX THE CONTENTS. BE SURE TO ROLL IT GENTLY BETWEEN YOUR HANDS; DO NOT SHAKE IT. THE REASON YOU DO NOT SHAKE INSULIN IS TO PREVENT FOAM FORMATION, WHICH WILL MAKE ACCURATE MEASURING DIFFICULT DUE TO THE TINY AIR BUBBLES. SOME INSULIN WILL HAVE A STRONG TENDENCY TO SETTLE OUT OF SUSPENSION. IF IT IS NOT SHAKEN PROPERLY, IT WILL NOT MIX WELL AND DOSING WILL BE INACCURATE.
“THE TRICK IS TO MIX IT VIGOROUSLY ENOUGH TO BLEND IT WITHOUT CREATING FOAM.”
THEREFORE, THE TRICK IS TO MIX IT VIGOROUSLY ENOUGH TO BLEND IT WITHOUT CREATING FOAM. WHEN YOU HAVE FINISHED MIXING THE INSULIN, TURN THE BOTTLE UPSIDE DOWN TO SEE IF ANY WHITE POWDER ADHERES TO THE BOTTOM OF THE BOTTLE. IF SO, MORE MIXING IS NEEDED.
HAVE THE NEEDLE AND SYRINGE, INSULIN BOTTLE, AND DOG READY. THEN, FOLLOW THESE STEPS:
1. REMOVE THE CAP FROM THE NEEDLE, AND DRAW BACK THE PLUNGER TO THE APPROPRIATE DOSE.
2. CAREFULLY INSERT THE NEEDLE INTO THE INSULIN BOTTLE.
3. INJECT AIR INTO THE BOTTLE. THIS PREVENTS A VACUUM FROM FORMING WITHIN THE BOTTLE.
4. WITHDRAW THE CORRECT AMOUNT OF INSULIN INTO THE SYRINGE.
IN ORDER TO ENSURE THAT YOU HAVE THE CORRECT AMOUNT OF INSULIN IN THE SYRINGE, MAKE SURE THAT IT STARTS AT THE “0” ON THE SYRINGE BARREL, AND THAT THE EDGE OF THE PLUNGER NEAREST THE NEEDLE IS ON THE CORRECT UNIT MARK ON THE BARREL.
BEFORE INJECTING YOUR DOG WITH THE INSULIN, CHECK THAT THERE ARE NO AIR BUBBLES IN THE SYRINGE. IF YOU GET AN AIR BUBBLE, DRAW TWICE AS MUCH INSULIN INTO THE SYRINGE AS YOU NEED. THEN WITHDRAW THE NEEDLE FROM THE INSULIN BOTTLE AND TAP THE SIDE OF THE BARREL OF THE SYRINGE WITH YOUR FINGERNAIL TO MAKE THE AIR BUBBLE RISE TO THE TIP OF THE SYRINGE. GENTLY AND SLOWLY EXPEL THE AIR BUBBLE BY MOVING THE PLUNGER UPWARD. WHEN YOU HAVE REMOVED ALL OF THE AIR BUBBLES, DOUBLE-CHECK THAT YOU HAVE THE CORRECT AMOUNT OF INSULIN IN THE SYRINGE.
HOW DO I INJECT THE INSULIN?
THE STEPS TO FOLLOW FOR INJECTING INSULIN IN YOUR DOG ARE:
1) HOLD THE SYRINGE IN YOUR RIGHT HAND (IF YOU ARE RIGHT-HANDED).
2) HAVE SOMEONE HOLD YOUR DOG WHILE YOU PICK UP A FOLD OF SKIN FROM SOMEWHERE ALONG YOUR DOG’S BACK IN THE “SCRUFF” REGION OF THE NECK WITH YOUR FREE HAND. TRY TO PICK UP A SLIGHTLY DIFFERENT SPOT EACH DAY.
3) QUICKLY PUSH THE VERY SHARP, VERY THIN NEEDLE THROUGH YOUR DOG’S SKIN AT ABOUT A FORTY-FIVE DEGREE ANGLE. THIS SHOULD BE FAST, EASY AND PAINLESS. HOWEVER, TAKE CARE TO PUSH THE NEEDLE THROUGH ONLY ONE LAYER OF SKIN AND NOT INTO YOUR FINGER OR THROUGH TWO LAYERS OF SKIN AND OUT THE OTHER SIDE. THE LATTER WILL RESULT IN INJECTING THE INSULIN ONTO YOUR DOG’S HAIRCOAT OR ONTO THE FLOOR. THE NEEDLE SHOULD BE DIRECTED PARALLEL TO THE BACKBONE OR ANGLED SLIGHTLY DOWNWARD.
4) TO INJECT THE INSULIN, PLACE YOUR THUMB ON THE PLUNGER AND PUSH IT ALL THE WAY INTO THE SYRINGE BARREL. IF YOU ARE UNSURE IF YOU ADMINISTERED IT CORRECTLY, OR IF YOU “MISSED,” DO NOT ADMINISTER ADDITIONAL INSULIN. SIMPLY RESUME YOUR NORMAL SCHEDULE AND GIVE THE NEXT INSULIN INJECTION AT THE REGULAR TIME.
5) WITHDRAW THE NEEDLE FROM YOUR DOG’S SKIN. IMMEDIATELY PLACE THE NEEDLE GUARD OVER THE NEEDLE AND PLACE THE USED NEEDLE AND SYRINGE INTO A PUNCTURE-RESISTANT CONTAINER. BE AWARE THAT SOME COMMUNITIES HAVE STRICT RULES ABOUT DISPOSAL OF MEDICAL WASTE MATERIAL SO DON’T THROW THE NEEDLE AND SYRINGE INTO THE GARBAGE UNTIL YOU KNOW IF THIS IS PERMISSIBLE. IT IS USUALLY PREFERABLE TO TAKE THE USED NEEDLES AND SYRINGES TO YOUR VETERINARY CLINIC OR LOCAL PHARMACY FOR DISPOSAL.
6) STROKE AND PRAISE YOUR DOG TO REWARD IT FOR SITTING QUIETLY.
SHOULD I STERILIZE THE SKIN WITH ALCOHOL BEFORE GIVING THE INJECTION?
IT IS NEITHER NECESSARY NOR DESIRABLE TO SWAB THE SKIN WITH ALCOHOL TO “STERILIZE” IT. THERE ARE FOUR REASONS:
1) THE STING CAUSED BY THE ALCOHOL CAN MAKE YOUR DOG DISLIKE THE INJECTIONS.
2) DUE TO THE NATURE OF THE THICK HAIR COAT AND THE TYPE OF BACTERIA THAT LIVE NEAR THE SKIN OF DOGS, BRIEF SWABBING WITH ALCOHOL OR ANY OTHER ANTISEPTIC IS NOT EFFECTIVE.
3) BECAUSE A SMALL AMOUNT OF ALCOHOL CAN BE CARRIED THROUGH THE SKIN BY THE NEEDLE, IT MAY ACTUALLY CARRY BACTERIA WITH IT INTO THE SKIN.
4) IF YOU HAVE ACCIDENTALLY INJECTED THE INSULIN ONTO THE SURFACE OF THE SKIN, YOU WILL NOT KNOW IT. IF YOU DO NOT USE ALCOHOL AND THE SKIN OR HAIR IS WET FOLLOWING AN INJECTION, THE INJECTION WAS NOT DONE PROPERLY.
ALTHOUGH THE ABOVE PROCEDURES MAY AT FIRST SEEM COMPLICATED AND SOMEWHAT OVERWHELMING, THEY WILL VERY QUICKLY BECOME SECOND NATURE. YOUR DOG WILL SOON LEARN THAT ONCE OR TWICE EACH DAY IT HAS TO SIT STILL FOR A FEW MINUTES. IN MOST CASES, A REWARD OF STROKING RESULTS IN A FULLY COOPERATIVE DOG THAT EVENTUALLY MAY NOT EVEN NEED TO BE HELD.
DOES HYPOGLYCEMIA OCCUR IN DOGS?
HYPOGLYCEMIA MEANS LOW BLOOD SUGAR. IF THE BLOOD SUGAR FALLS BELOW 40 MG/DL, IT CAN BE LIFE THREATENING. HYPOGLYCEMIA GENERALLY OCCURS UNDER TWO CONDITIONS:
“IT IS POSSIBLE FOR THE DOG’S INSULIN REQUIREMENTS TO SUDDENLY CHANGE.”
1) WHEN THE INSULIN DOSE IS TOO HIGH. ALTHOUGH MOST DOGS WILL REQUIRE THE SAME DOSE OF INSULIN FOR LONG PERIODS OF TIME, IT IS POSSIBLE FOR THE DOG’S INSULIN REQUIREMENTS TO SUDDENLY CHANGE. HOWEVER, THE MOST COMMON CAUSES FOR CHANGE ARE A REDUCTION IN FOOD INTAKE AND AN INCREASE IN EXERCISE OR ACTIVITY. THE DOG SHOULD EAT BEFORE GIVING THE INSULIN INJECTION, BECAUSE ONCE THE INSULIN IS ADMINISTERED IT CAN’T BE REMOVED FROM THE BODY. IF YOUR DOG DOES NOT EAT, SKIP THAT DOSE OF INSULIN. IF ONLY HALF OF THE FOOD IS EATEN, GIVE ONLY A HALF DOSE OF INSULIN. ALWAYS REMEMBER THAT IT IS BETTER IN THE SHORT TERM FOR THE BLOOD SUGAR TO BE TOO HIGH THAN TOO LOW.
2) WHEN TOO MUCH INSULIN IS GIVEN. THIS CAN OCCUR BECAUSE THE INSULIN WAS NOT PROPERLY MEASURED IN THE SYRINGE OR BECAUSE TWO DOSES WERE GIVEN. YOU MAY FORGET THAT YOU GAVE IT AND REPEAT IT, OR TWO PEOPLE IN THE FAMILY MAY EACH GIVE A DOSE. A CHART TO RECORD INSULIN ADMINISTRATION WILL HELP TO PREVENT THE DOG BEING TREATED TWICE.
THE MOST LIKELY TIME THAT A DOG WILL BECOME HYPOGLYCEMIC IS THE TIME OF PEAK INSULIN EFFECT (5-8 HOURS AFTER AN INSULIN INJECTION). WHEN THE BLOOD GLUCOSE IS ONLY MILDLY LOW, THE DOG WILL ACT VERY TIRED AND UNRESPONSIVE. YOU MAY CALL IT AND GET LITTLE OR NO RESPONSE. WITHIN A FEW HOURS, THE BLOOD GLUCOSE WILL RISE, AND YOUR DOG WILL RETURN TO NORMAL. SINCE MANY DOGS SLEEP A LOT DURING THE DAY, THIS IMPORTANT SIGN IS EASILY MISSED. WATCH FOR ANY SUBTLE SIGNS OF HYPOGLYCEMIA. IT IS THE FIRST SIGN OF IMPENDING PROBLEMS. IF YOU SEE IT, PLEASE BRING YOUR DOG IN FOR BLOOD GLUCOSE TESTING.
IF YOUR DOG IS SLOW TO RECOVER FROM THIS PERIOD OF LETHARGY, YOU SHOULD GIVE IT CORN SYRUP (ONE TABLESPOON FOR EVERY TWENTY POUNDS (APPROXIMATELY 15 ML/10 KG) BY MOUTH). IF THERE IS NO RESPONSE WITHIN FIFTEEN MINUTES, REPEAT ADMINISTRATION OF THE CORN SYRUP. IF THERE IS STILL NO RESPONSE, CONTACT YOUR VETERINARIAN IMMEDIATELY FOR FURTHER INSTRUCTIONS. THIS IS AN EMERGENCY.
IF SEVERE HYPOGLYCEMIA OCCURS, A DOG MAY HAVE SEIZURES OR LOSE CONSCIOUSNESS. ULTIMATELY, UNTREATED HYPOGLYCEMIA WILL LEAD TO COMA AND DEATH. THIS IS AN EMERGENCY THAT CAN ONLY BE REVERSED WITH INTRAVENOUS ADMINISTRATION OF GLUCOSE. IF IT OCCURS DURING OFFICE HOURS, TAKE YOUR DOG TO THE VETERINARIAN’S OFFICE IMMEDIATELY. IF IT OCCURS AT NIGHT OR ON THE WEEKEND, CALL YOUR VETERINARIAN’S EMERGENCY PHONE NUMBER FOR INSTRUCTIONS.
SUMMARY OF INSTRUCTIONS FOR INSULIN TREATMENT OF YOUR DOG:
READ AND REREAD THIS MATERIAL SO THAT YOU UNDERSTAND THE SPECIFICS OF PROPER REGULATION AND HOW TO RECOGNIZE AND TREAT HYPOGLYCEMIA.
PURCHASE THE SUPPLIES FOR TREATMENT. YOUR PRESCRIPTION WILL SPECIFY THE TYPE OF INSULIN AND SYRINGES. IF YOU WILL BE USING URINE GLUCOSE TESTS STRIPS, THEY SHOULD BE PURCHASED AT A PHARMACY.
TYPE OF INSULIN:
TYPE OF INSULIN SYRINGES: ___U-100 ___U-40
GIVE THE FIRST INJECTION OF INSULIN OF _____UNITS AT ABOUT _________ AM / PM.
___IF YOUR DOG SHOWS SYMPTOMS OF LOW BLOOD SUGAR, GIVE ______________ TBSP (______MLS) OF CORN SYRUP, BASED ON YOUR DOG’S BODY WEIGHT OF ____________.
___RETURN FOR A GLUCOSE CURVE, NO LATER THAN ________ A.M., ON ____________. FEED YOUR DOG THAT MORNING AND IMMEDIATELY BRING IT TO THE HOSPITAL. DO NOT GIVE INSULIN, BUT BRING IT WITH YOU. (IF IT WILL TAKE MORE THAN 30MINUTES TO DRIVE TO THE HOSPITAL, CALL FOR INSTRUCTIONS ON FEEDING.)
___FOLLOWING REGULATION IN THE HOSPITAL, MEASURE THE URINE GLUCOSE TWO CONSECUTIVE DAYS, THEN TWICE WEEKLY FOR THE NEXT TWO WEEKS. IF GLUCOSE IS NOT DETECTED, MEASURE THE GLUCOSE TWO CONSECUTIVE DAYS EVERY OTHER WEEK OR AS DIRECTED.
___IF YOU ARE UNABLE TO TEST THE URINE FOR GLUCOSE, RETURN TO OUR HOSPITAL IN TWO TO FOUR DAYS FOR A BLOOD GLUCOSE TEST. THIS IS OFTEN PERFORMED ABOUT FIVE TO EIGHT HOURS AFTER AN INJECTION OF INSULIN. IF TWO INJECTIONS ARE GIVEN EACH DAY, BE SURE THE TEST IS DONE BEFORE THE EVENING INJECTION. DATE AND TIME TO RETURN: ___________________________________ AM / PM
___RETURN TO OUR HOSPITAL FOR A BLOOD GLUCOSE TEST IN ONE MONTH. THIS SHOULD BE DONE ABOUT FIVE TO EIGHT HOURS AFTER AN INJECTION OF INSULIN. IF TWO INJECTIONS ARE GIVEN EACH DAY, BE SURE THE TEST IS DONE BEFORE THE EVENING INJECTION.
___RETURN TO OUR HOSPITAL FOR A FRUCTOSAMINE TEST IN ONE MONTH. FOR THIS TEST, THE TIME OF DAY IS NOT IMPORTANT AND FASTING IS NOT NECESSARY.
THIS CLIENT INFORMATION SHEET IS BASED ON MATERIAL
WRITTEN BY: ERNEST WARD, DVM
DID YOU KNOW THAT DOGS ALMOST EXCLUSIVELY HAVE TYPE 1 DIABETES?
NIPPING FERRET? TRY THESE TRAINING TIPS TO SOLVE YOUR FERRET’S BEHAVIOR PROBLEMS.
IS YOUR FERRET LOSING HAIR? THIS DISEASE COULD BE THE REASON.
FACT: FERRETS CAN EAT 7 TO 10 SMALL MEALS A DAY.
PETS CANNOT SPEAK, BUT THEY CAN COMMUNICATE. UNDERSTAND WHEN THEY ARE IN PAIN.
BEARDED DRAGONS CAN LIVE UP TO 12 YEARS WHEN PROPERLY CARED FOR. DO YOU KNOW THE FACTS?
WASHING YOUR HANDS IS JUST ONE WAY TO AVOID THIS SERIOUS DISEASE.
THE TRUTH ABOUT WORKING IN A VETERINARIAN’S OFFICE.
WHEEZING IS A SIGN OF THIS IRREVERSIBLE DISEASE.
THIS HIGHLY CONTAGIOUS CONDITION IN DOGS CAN BE PREVENTED.
IGNORING THIS CONDITION IN YOUR PET COULD LEAD TO BLINDNESS.
“IF YOU HEAR YOUR DOG YELP, HE MAY NEED YOUR HELP.”
ARTHRITIS IN CATS
MARCH 19, 2014
FELINE ARTHRITIS CAN BE CAUSED BY INJURY, INFECTION, AN AUTOIMMUNE DISORDER, OR DEGENERATIVE PROBLEMS INVOLVING THE JOINTS. IF A CAT SEEMS STIFF OR PAINFUL, HAS SWOLLEN JOINTS, LOSES MUSCLE MASS, OR HAS A HARD TIME MOVING AROUND, IT MIGHT HAVE ARTHRITIS. KEEPING A CAT IN GOOD SHAPE THROUGH PROPER DIET CAN HELP RELIEVE THE SYMPTOMS. MEDICATIONS AND SUPPLEMENTS CAN HELP, AS CAN MASSAGE, ACUPUNCTURE, AND EVEN SURGERY.
OVERVIEW
MOST CAT OWNERS THINK ARTHRITIS IS A DISEASE FOR DOGS. THEY DON’T NECESSARILY LOOK OUT FOR ITS SIGNS. IN FACT, BY THE TIME MOST CAT OWNERS NOTICE SOMETHING IS WRONG THEY HAVE A HARD TIME BELIEVING THAT THE LOSS OF MUSCLE AND FUNCTION IS THE RESULT OF ARTHRITIS. THAT IS WHY SO MANY CAT OWNERS TEND TO GET A LATE START ON TREATING THE DISEASE.
ARTHRITIS IS A JOINT PROBLEM THAT CAN REDUCE MOBILITY AND ELICIT PAIN. IT CAN BE CAUSED BY INJURY, INFECTION, THE BODY’S OWN IMMUNE SYSTEM, OR DEVELOPMENTAL PROBLEMS INVOLVING THE JOINTS.
HOWEVER, THE MOST COMMON FORM OF ARTHRITIS IN CATS IS CALLED OSTEOARTHRITIS OR DEGENERATIVE JOINT DISEASE. NORMALLY, JOINTS FORM SMOOTH CONNECTIONS BETWEEN BONES, BUT IN THE CASE OF OSTEOARTHRITIS, THAT SMOOTH, GLISTENING SURFACE ON THE END OF A BONE IS TRANSFORMED INTO A ROUGHENED, POORLY GLIDING SURFACE.
OSTEOARTHRITIS INVOLVES THE THINNING OF JOINT CARTILAGE (A PROTECTIVE CUSHIONING BETWEEN BONES), THE BUILDUP OF FLUID WITHIN THE JOINT, AND, ULTIMATELY, THE FORMATION OF BONY GROWTHS WITHIN THE JOINT. OVER TIME, THE ROUGHNESS CREATED BY THESE BONY GROWTHS CAN LEAD TO REDUCED JOINT MOBILITY AND PAIN — EVEN IN CATS.
SYMPTOMS AND IDENTIFICATION
SIGNS OF ARTHRITIS INCLUDE:
STIFFNESS AFTER EXERCISE
WASTING AWAY OF MUSCLE
LIMITED MOVEMENT
JOINT SWELLING
TROUBLE GETTING UP, LYING DOWN, WALKING, CLIMBING STAIRS, OR JUMPING
A GRATING SOUND IN A JOINT
RECOGNIZING ARTHRITIS IN CATS CAN BE DIFFICULT BECAUSE THE CONDITION PROGRESSES SLOWLY AND CATS DON’T COMPLAIN ABOUT THEIR ACHING JOINTS. ALSO, SOME OWNERS ASSUME THAT SIGNS OF ARTHRITIS (SLOWING DOWN AND STIFFNESS, PRIMARILY) ARE “NORMAL” IN OLDER ANIMALS.
TAKING A CAT IN FOR REGULAR CHECKUPS CAN HELP A VETERINARIAN IDENTIFY CLINICAL SIGNS EARLY. RADIOGRAPHY (X-RAYS) CAN REVEAL BONY GROWTHS AND JOINT ABNORMALITIES.
AFFECTED BREEDS
ANY CAT CAN DEVELOP ARTHRITIS.
TREATMENT
THESE APPROACHES ARE COMMONLY RECOMMENDED FOR THE TREATMENT OF ARTHRITIS IN CATS:
GETTING OR KEEPING CATS SLIM CAN HELP BY DECREASING THE LOAD ON THEIR JOINTS.
FEEDING CATS THE RIGHT AMOUNT OF HIGH-QUALITY FOOD SHOULD HELP WITH WEIGHT CONTROL.
CAREFULLY MONITORED EXERCISE ON SOFT SURFACES CAN HELP AFFECTED CATS. BECAUSE ARTHRITIS IS AGGRAVATED BY THE COLD AND DAMP, AFFECTED CATS SHOULD BE KEPT WARM AND DRY. PADDED CAT BEDS CAN HELP.
WARM COMPRESSES CAN SOOTHE AFFECTED JOINTS.
MASSAGE CAN INCREASE A CAT’S FLEXIBILITY, CIRCULATION, AND SENSE OF WELL-BEING. PROFESSIONAL ANIMAL MASSAGE THERAPISTS ARE AVAILABLE.
PAIN MEDICATION, INCLUDING NON-STEROIDAL ANTI-INFLAMMATORY DRUGS (COMMONLY CALLED NSAIDS), MAY HELP RELIEVE SIGNS.
CORTICOSTEROIDS CAN BE USED TO SUPPRESS INFLAMMATION, BUT THEY ARE USUALLY USED FOR SHORT PERIODS ONLY.
DISEASE-MODIFYING OSTEOARTHRITIS DRUGS (DMOADS) CAN BE AN IMPORTANT PART OF MANAGING OSTEOARTHRITIS.
GLUCOSAMINE AND CHONDROITIN NUTRITIONAL SUPPLEMENTS HAVE BEEN USED TO HELP MANAGE ARTHRITIS IN FELINES.
ACUPUNCTURE ISN’T JUST FOR PEOPLE. IT’S PAINLESS AND MAY HELP CATS, TOO.
SURGERY MAY BE A GOOD CHOICE IN ADVANCED CASES OF FELINE ARTHRITIS. A LOW-STRESS ENVIRONMENT, PLENTY OF AFFECTION, AND SUPPORTIVE CARE CAN HELP IMPROVE ANY CAT’S QUALITY OF LIFE.
PREVENTION
WITH MANY PET CATS LIVING WELL INTO THEIR TEENS AND EVEN EARLY 20S, MOST CASES OF OSTEOARTHRITIS IN CATS ARE PROBABLY NOT PREVENTABLE. BUT REGULAR, MODERATE EXERCISE AND A HIGH-QUALITY DIET CAN HELP MANAGE BODY WEIGHT AND HELP KEEP A CAT’S MUSCULOSKELETAL SYSTEM IN EXCELLENT SHAPE.
AS PETS AGE, OSTEOARTHRITIS CAN APPEAR GRADUALLY WITH VERY SUBTLE SIGNS. REGULAR VETERINARY VISITS PROVIDE A GREAT OPPORTUNITY TO ASSESS YOUR CAT’S JOINT HEALTH, GET A DIAGNOSIS EARLY DURING THE COURSE OF DISEASE, AND START INSTITUTING CHANGES TO MAKE YOUR CAT COMFORTABLE AND IMPROVE HIS QUALITY OF LIFE.
THIS ARTICLE HAS BEEN REVIEWED BY A VETERINARIAN.
HELPING YOUR DOG WITH OSTEOARTHRITIS
A DIAGNOSIS OF OSTEOARTHRITIS (OA) IN YOUR DOG CAN FEEL DEVASTATING AND EVEN OVERWHELMING. AFTER ALL, WE KNOW THAT OA IS A PROGRESSIVE, DEGENERATIVE DISEASE THAT WILL WORSEN OVER TIME. BY MOST ESTIMATES, 20% OF ALL DOGS (REGARDLESS OF AGE) ARE AFFECTED BY OA, MAKING IT THE MOST COMMON CHRONIC DISEASE THEY FACE. ONCE A DOG IS DIAGNOSED WITH OA, IT IS IMPORTANT TO UNDERSTAND THAT OUR FOCUS IS MANAGEMENT RATHER THAN CURE. SUCCESS MEANS MAXIMIZING YOUR DOG’S COMFORT AND FUNCTION WHILE MINIMIZING PAIN.
SUCCESSFULLY MANAGING YOUR DOG’S OA MEANS MAXIMIZING COMFORT AND FUNCTION WHILE MINIMIZING PAIN.
THE GOOD NEWS IS THAT THERE ARE MANY STRATEGIES, BOTH BIG AND SMALL, TO HELP DOGS LIVE WITH THEIR OA.
WHAT IS THE FIRST STEP I SHOULD TAKE TO HELP MY DOG WITH OA?
CREATE A TRUE PARTNERSHIP WITH YOUR VETERINARIAN. THIS MEANS SCHEDULING REGULAR EVALUATIONS TO MONITOR THE PROGRESSION OF OA AND MODIFY THE TREATMENT PLAN. DEDICATE A JOURNAL OR NOTEBOOK TO YOUR DOG’S ONGOING HEALTH/MEDICAL ISSUES, AND WRITE DOWN ALL YOUR QUESTIONS AS YOU THINK OF THEM. TAKE YOUR NOTEBOOK TO ALL VETERINARY VISITS TO RECORD ANSWERS TO YOUR QUESTIONS AS WELL AS TO NOTE THE DETAILS OF ANY UPDATED VETERINARY RECOMMENDATIONS. WE ONLY RECALL ABOUT 10% OF WHAT WE HEAR, SO IT MAKES SENSE TO WRITE THINGS DOWN.
CAN MY DOG’S WEIGHT MAKE A DIFFERENCE IN MANAGING OA?
YES, IT CAN. IF YOUR DOG IS CARRYING EXTRA WEIGHT, WORK WITH YOUR VETERINARIAN TO PLAN A WEIGHT-LOSS STRATEGY TO GET YOUR DOG LEAN AND KEEP HIM OR HER THAT WAY. YOUR VETERINARIAN WILL PRESCRIBE A DIET THAT WILL PROVIDE JOINT SUPPORT AND HELP YOUR DOG LOSE WEIGHT. ASK FOR SPECIFIC PORTION RECOMMENDATIONS, AND SCHEDULE REGULAR WEIGH-INS TO MONITOR SUCCESS.
CAN EXERCISE HELP?
WITH OA JOINTS, WE KNOW THAT DOGS NEED TO “USE IT OR LOSE IT.” REGULAR MODERATE EXERCISE CONTRIBUTES TO BETTER JOINT HEALTH, EVEN IN THE FACE OF OA. ASK YOUR VETERINARIAN FOR SPECIFIC GUIDANCE ON HOW FAR AND LONG TO WALK, ACCEPTABLE WALKING SURFACES, AND SPECIFIC EXERCISES THAT CAN TARGET AND STRENGTHEN MUSCLE GROUPS.
IS THERE ANYTHING I SHOULD KNOW ABOUT THE PAIN MEDICATIONS/NUTRACEUTICALS/SUPPLEMENTS MY VETERINARIAN HAS PRESCRIBED FOR MY DOG?
USE ALL PRODUCTS STRICTLY AS INSTRUCTED/LABELED. DO NOT MODIFY DELIVERY/DOSING OF PRESCRIPTION MEDICATIONS EXCEPT UNDER THE DIRECTION OF YOUR VETERINARIAN. BE SURE TO ASK FOR A WRITTEN SUMMARY OF POTENTIAL SIDE EFFECTS, AND MONITOR YOUR DOG CAREFULLY. IF YOU WITNESS ANY ADVERSE SIDE EFFECTS FROM MEDICATIONS, CONTACT YOUR VETERINARIAN IMMEDIATELY.
ARE THERE ANY OTHER VETERINARY MANAGEMENT OPTIONS I CAN LOOK INTO?
YOU MAY WANT TO EXPLORE PHYSICAL MEDICINE TO COMPLEMENT MEDICATION, NUTRITION, AND NUTRACEUTICALS TO HELP YOUR DOG WITH OA. PHYSICAL MEDICINE OPTIONS INCLUDE PHYSICAL REHABILITATION, ACUPUNCTURE, CHIROPRACTIC, AND MEDICAL MASSAGE. YOU WANT TO WORK WITH APPROPRIATELY QUALIFIED AND CREDENTIALED INDIVIDUALS, SO SEEK YOUR VETERINARIAN’S GUIDANCE FOR A REFERRAL. PHYSICAL MEDICINE MAY ALLOW FOR DECREASED DOSES OF MEDICATION OVER TIME BY HELPING TO RESTORE MORE NORMAL BIOMECHANICS, MOVEMENT, AND STRENGTH IN THE DOG’S BODY.
PHYSICAL MEDICINE MAY HELP RESTORE MORE NORMAL BIOMECHANICS, MOVEMENT, AND STRENGTH IN YOUR DOG’S BODY.
HOW CAN I MODIFY MY HOME ENVIRONMENT TO MAXIMIZE MY DOG’S COMFORT AND FUNCTION?
THERE ARE SOME SIMPLE THINGS YOU CAN DO TO MAKE EVERYDAY LIVING MUCH MORE COMFORTABLE AND FUN FOR YOUR DOG WITH OA. SOMETHING AS STRAIGHTFORWARD AS PROVIDING RAISED FOOD AND WATER DISHES CAN RELIEVE LOW-BACK PAIN AND MAKE MEALTIMES MORE ENJOYABLE. DISHES BETWEEN YOUR DOG’S ELBOW AND SHOULDER LEVEL ARE GENERALLY MOST CONVENIENT.
 IN ADDITION, KEEP YOUR DOG WITH OA WARM AND DRY. OUTDOOR LIVING IS, IN GENERAL, NOT APPROPRIATE FOR THESE DOGS. TO MAKE SLEEPING SURFACES AS COMFORTABLE AS POSSIBLE, CONSIDER PROVIDING YOUR DOG WITH AN ORTHOPEDIC OR MEMORY FOAM BED.
IN ADDITION, KEEP YOUR DOG WITH OA WARM AND DRY. OUTDOOR LIVING IS, IN GENERAL, NOT APPROPRIATE FOR THESE DOGS. TO MAKE SLEEPING SURFACES AS COMFORTABLE AS POSSIBLE, CONSIDER PROVIDING YOUR DOG WITH AN ORTHOPEDIC OR MEMORY FOAM BED.
A RAMP TO ENTER AND LEAVE THE VEHICLE MAKES CAR RIDES MORE ENJOYABLE BY ELIMINATING STRESS ON THE BACK AND LEG JOINTS. DOGS GENERALLY LEARN HOW TO USE RAMPS QUICKLY.
DEPENDING ON THE EXTENT OF YOUR DOG’S OA, IT MAY BE BEST TO PREVENT ACCESS TO STAIRS WHEN NO ONE IS AVAILABLE TO “SPOT” THE DOG ON A TRIP UPSTAIRS OR DOWNSTAIRS. A COLLAPSIBLE BABY GATE WORKS GREAT FOR THIS AND CAN EITHER BE MOUNTED ON HINGES OR SIMPLY PUT UP AND REMOVED AS NEEDED.
AN OFTEN-OVERLOOKED YET VERY IMPORTANT ENVIRONMENTAL MODIFICATION IS SLIP-FREE FLOORING.
FINALLY, AN OFTEN-OVERLOOKED YET VERY IMPORTANT ENVIRONMENTAL MODIFICATION IS SLIP-FREE FLOORING. IN THIS AGE OF HARDWOOD, LAMINATE, TILE, AND VINYL FLOORING, MOST DOGS WITH OA ARE SIMPLY DOOMED TO STRUGGLE JUST TO GET AROUND THE HOUSE. WE CAN HELP THEM OUT IN A NUMBER OF WAYS:
- ADDING AREA RUGS WITH NON-SKID BACKING.
- USING BABY GATES TO PREVENT ACCESS TO ROOMS WITH SLICK FLOORS.
- LAYING DOWN INTERLOCKING SQUARES OF LIGHTLY PADDED FLOORING (SUCH AS THOSE USED TO CREATE PLAY SURFACES FOR CHILDREN). THESE SQUARES WORK WELL FOR COVERING LARGE FLOOR SURFACES BECAUSE THEY CAN BE CUSTOM-FITTED TO ANY ROOM AND EASILY
- REMOVED FOR CLEANING AND ENTERTAINING COMPANY.
WHAT IS MY TAKEAWAY MESSAGE?
WORK WITH YOUR VETERINARIAN TO EXPAND AND FINE-TUNE THESE OPTIONS FOR YOUR DOG. WITH A BIT OF IMAGINATION AND CREATIVE THOUGHT, YOU CAN HELP YOUR DOG WITH OA ENJOY A LONG, HAPPY, AND COMFORTABLE LIFE!
THIS CLIENT INFORMATION SHEET IS BASED ON MATERIAL
WRITTEN BY: ROBIN DOWNING, DVM, CVPP, CCRP, DAAPM
PUPPIES AS YOUNG AS FIVE MONTHS CAN DEVELOP HIP DYSPLASIA.
CHECK OUT THESE TIPS AND TRICKS FOR TRAINING YOUR BIRD!
FEATHER PLUCKING: MALNUTRITION OR SOMETHING ELSE?
DO YOU KNOW HOW OFTEN YOU SHOULD FEED YOUR BIRD FRUITS AND VEGETABLES?
FROM TEMPERATURE TO TOYS: MAKE SURE YOUR BIRD’S BASIC NEEDS ARE BEING MET.
DO YOU KNOW WHY YOUR CAT’S NUTRITION IS SO IMPORTANT?
UNDERSTAND WHY YOUR CAT MAY BE URINATING OUTSIDE THE BOX AND WHAT YOU CAN DO TO HELP.
FACT: KIDNEY DISEASE IS ONE OF THE MOST COMMON CONDITIONS IN CATS.
WHAT ARE SOME OF THE COMMON DISEASES OF PET RABBITS?
COMMON CONDITIONS OF PET RABBITS INCLUDE SNUFFLES, INTERNAL AND EXTERNAL PARASITES, OVERGROWN INCISORS, UTERINE PROBLEMS (INFECTIONS OR CANCER), AND SORE HOCKS.
WHAT ARE THE SIGNS OF THESE DISEASES?
“SNUFFLES” IS THE LAY TERM GIVEN TO AN INFECTION OF THE UPPER RESPIRATORY TRACT GENERALLY CAUSED BY SPECIES OF BACTERIA CALLED PASTEURELLA MULTOCIDA.(ALTHOUGH OTHER BACTERIA CAN ALSO CAUSE THIS INFECTION). MOST COMMONLY, CLINICAL SIGNS ARE RELATED TO THE EYES (MUCOID OR PURULENT DISCHARGE, REDNESS, SQUINTING) OR NOSE AND SINUSES (SNEEZING, MUCOID OR PURULENT DISCHARGE). OFTEN THE EYES AND NOSE ARE AFFECTED AT THE SAME TIME. CRUSTY, MATTED FUR IS OFTEN SEEN ON THE INSIDE OF THE FRONT PAWS. PASTEURELLA MULTOCIDA CAN INFECT OTHER AREAS OF THE BODY AS WELL. EAR INFECTIONS (RESULTING IN A HEAD TILT), ABSCESSES (SEEN AS LUMPS ON THE BODY), AND UTERINE INFECTIONS (OFTEN ONLY DIAGNOSED DURING EXPLORATORY SURGERY) ARE FREQUENTLY SEEN. SUDDEN DEATH FROM SEPTICEMIA (INFECTION IN THE BLOOD) IS RARE BUT CAN OCCUR.
RABBITS CAN BECOME INFECTED WITH VARIOUS INTESTINAL PARASITES (COCCIDIA AND PINWORMS ARE COMMON), AS WELL AS EXTERNAL PARASITES SUCH AS EAR AND FUR MITES, FLEAS AND OCCASIONALLY TICKS. REGULAR EXAMINATIONS INCLUDING MICROSCOPIC FECAL EXAMINATIONS (AT LEAST ONCE A YEAR) WILL ALLOW EASY DIAGNOSIS AND TREATMENT.
A RABBIT’S TEETH ARE CONTINUOUSLY GROWING BUT THE DAILY ACT OF CHEWING FOOD AS WELL AS CHEWING ON WOODEN BLOCKS, BRANCHES AND TOYS HELPS THEM WEAR DOWN AT A RATE EQUAL TO THEIR GROWTH. REGULAR CHEWING EXERCISE KEEPS THE TEETH AT A CONSISTENT NORMAL, FUNCTIONAL LENGTH. OCCASIONALLY, TRAUMA OR DISEASE WILL CHANGE THE WAY THE TEETH GROW AND THEY WILL BECOME OVERGROWN. BOTH THE MOLARS AND THE INCISORS (THE BIG TEETH YOU CAN SEE AT THE FRONT OF THE MOUTH) CAN BE AFFECTED, BUT THE INCISORS ARE MORE OFTEN THE PROBLEM. RABBITS WITH OVERGROWN TEETH MAY STOP EATING AND DROOL EXCESSIVELY. YOU CAN EASILY DETECT A PROBLEM WITH THE INCISORS BY LOOKING INTO THE RABBIT’S MOUTH. A VETERINARIAN FAMILIAR WITH RABBITS WILL HAVE TO ASSESS THE MOLARS, WHICH ARE FURTHER BACK IN THE MOUTH.
LIKE DOGS AND CATS, FEMALE RABBITS SHOULD BE SPAYED EARLY IN LIFE (BY 4-6 MONTHS OF AGE). UN-SPAYED FEMALE DOGS AND CATS OFTEN DEVELOP MALIGNANT BREAST CANCER, UN-SPAYED FEMALE FERRETS CAN DIE OF FATAL ANEMIA, WHILE UN-SPAYED FEMALE RABBITS OFTEN DEVELOP UTERINE CANCER. THIS TYPE OF CANCER IS CALLED UTERINE ADENOCARCINOMA AND IS A RELATIVELY COMMON CONDITION OF OLDER INTACT FEMALE RABBITS. IT SHOULD BE SUSPECTED ANYTIME AN UN-SPAYED FEMALE RABBIT BECOMES SICK OR IS PASSING BLOOD. DIAGNOSIS IS DIFFICULT AND OFTEN ONLY MADE DEFINITIVELY DURING EXPLORATORY SURGERY.
“UN-SPAYED FEMALE RABBITS OFTEN DEVELOP UTERINE CANCER.”
“SORE HOCKS” OR PODODERMATITIS IS A CONDITION THAT IS FAIRLY COMMON IN RABBITS. THE HOCKS ARE ESSENTIALLY THE ANKLES OF RABBITS. WHEN A RABBIT IS SITTING, WHICH IT DOES MOST OF THE TIME, ITS HOCKS ARE IN CONTACT WITH THE FLOOR OF ITS CAGE. OFTEN, WIRE-FLOORED CAGES ARE TOO ROUGH ON THE HOCKS, CAUSING THE PROTECTIVE FUR LAYER ON THE SOLE OF THE FOOT AND THE HOCK TO WEAR THIN; THE SKIN TURNS RED, EVENTUALLY WEARS THROUGH AND BECOMES ULCERATED AND PAINFUL. THE CONDITION IS USUALLY PREVENTED BY TAKING THE RABBIT OFF WIRE BOTTOM CAGES ENTIRELY OR FOR RABBITS THAT MUST LIVE IN WIRE CAGES, PROVIDE WITH ANOTHER SURFACE TO SIT ON, SUCH AS A PIECE OF WOOD, PLEXIGLAS, OR A TOWEL THAT COVERS AT LEAST HALF OF THE WIRE CAGE.
HOW CAN I TELL IF MY RABBIT IS SICK?
SOME SIGNS OF DISEASE IN RABBITS MAY BE SPECIFIC FOR A CERTAIN DISEASE. MORE COMMONLY, HOWEVER, SIGNS ARE VAGUE AND NON-SPECIFIC, SUCH AS A RABBIT WITH ANOREXIA (LACK OF APPETITE) AND LETHARGY, WHICH CAN BE SEEN WITH MANY DISEASES INCLUDING HAIRBALLS, UTERINE CANCER, AND EVEN KIDNEY OR LIVER FAILURE.
“IF A RABBIT MISSES EVEN ONE MEAL THIS IS A CAUSE FOR CONCERN AND SHOULD BE PROMPTLY INVESTIGATED.”
YOU SHOULD BE CONCERNED IF YOU NOTICE ANY DEVIATION FROM NORMAL, AND SHOULD IMMEDIATELY TAKE YOUR RABBIT TO YOUR VETERINARIAN FOR AN EVALUATION. IF A RABBIT MISSES EVEN ONE MEAL THIS IS A CAUSE FOR CONCERN AND SHOULD BE PROMPTLY INVESTIGATED.
HOW ARE RABBIT DISEASES TREATED?
MOST CASES OF SNUFFLES ARE MILD AND, IF CAUGHT EARLY, CAN BE MANAGED OR CURED. IF LEFT UNTREATED OR IF THE STRAIN OF BACTERIA IS PARTICULARLY AGGRESSIVE, THIS DISEASE CAN BE SEVERE, CHRONIC AND POTENTIALLY FATAL. A SWAB FOR BACTERIAL CULTURE CAN BE TAKEN TO HELP GUIDE TREATMENT. TREATMENT USUALLY INVOLVES EITHER ORAL OR INJECTABLE ANTIBIOTICS, GIVEN FOR A MINIMUM OF 2 – 4 WEEKS. IN SOME CASES, TREATMENT CAN BE REQUIRED FOR MONTHS (OR RARELY FOR YEARS) DEPENDING ON THE RESPONSE TO THERAPY. CERTAIN ORAL ANTIBIOTICS, ESPECIALLY ORAL PENICILLIN AND SIMILAR DRUGS, CAN BE FATAL TO RABBITS. THERE ARE SOME EXCELLENT ORAL AND INJECTABLE ANTIBIOTICS FOR USE IN RABBITS WITH THIS INFECTION, BUT NONE IS A SURE CURE. EYE DROPS AND NOSE DROPS , MAY BE USED IN CONJUNCTION WITH OTHER ANTIBIOTICS AS PRESCRIBED BY YOUR VETERINARIAN.
ALL RABBITS CARRY SOME PASTEURELLA ORGANISMS, BUT ONLY SOME SHOW OR MANIFEST DISEASE (THE IMMUNE SYSTEM GENERALLY KEEPS THE ORGANISMS IN CHECK). STRESSES SUCH AS IMPROPER DIET, NEW DIET, CHANGE IN DIET, INTRODUCTION OF A NEW PET, OVERCROWDING, ENVIRONMENTAL STRESSES, IMMUNOSUPPRESSION OR OTHER DISEASE MAY TRIGGER CLINICAL DISEASE. MANY RABBITS BECOME CHRONICALLY INFECTED. THE DISEASE IS EASILY TRANSMITTED BY CLOSE CONTACT BETWEEN RABBITS BUT REMEMBER THAT NOT ALL RABBITS WILL MANIFEST DISEASE. IDEALLY, NEW RABBITS SHOULD BE ISOLATED (FOR ABOUT ONE MONTH) BEFORE INTRODUCING THEM TO EXISTING PETS. LITTER SHOULD BE CHANGED REGULARLY TO PREVENT AMMONIA ACCUMULATION FROM THE URINE, WHICH CAN IRRITATE THE EYES AND NASAL TISSUE. RELAPSES MAY OCCUR IF YOUR RABBIT IS EXPOSED TO STRESSFUL SITUATIONS. IT IS IMPORTANT TO KEEP YOUR RABBIT AS HEALTHY AS POSSIBLE, TO MINIMIZE PROBLEMS WITH PASTEURELLOSIS.
EXTERNAL AND INTERNAL PARASITES ARE USUALLY TREATED EASILY. THE CHOICE OF MEDICATION YOUR VETERINARIAN WILL PRESCRIBE DEPENDS UPON THE FINDINGS OF AN EXAMINATION AND ANY NECESSARY ANCILLARY TESTS, SUCH AS A FECAL EXAMINATION FOR INTESTINAL PARASITES OR MICROSCOPIC EXAMINATION OF A SKIN SAMPLE OR AN EAR SWAB FOR EAR MITES. ORAL MEDICATIONS ARE USUALLY GIVEN FOR INTERNAL PARASITES. ORAL MEDICATION, TOPICAL MEDICATION, SHAMPOOS AND/OR ENVIRONMENTAL TREATMENTS MAY BE NECESSARY FOR EXTERNAL PARASITES, DEPENDING ON THE DIAGNOSIS. ONE SKIN MITE, CALLED CHEYLETIELLA OR WALKING DANDRUFF, CAN BE VERY CHALLENGING TO ELIMINATE.
OVERGROWN INCISORS OR MOLARS CAN BE MANAGED BY FILING OR GRINDING DOWN THE INCISORS, USUALLY UNDER ANESTHESIA. THIS TOOTH TRIMMING OFTEN HAS TO BE REPEATED AT REGULAR INTERVALS, AS THE TEETH CONTINUE TO GROW THROUGHOUT THE RABBIT’S LIFE. CLIPPING THE TEETH WITH NAIL TRIMMERS OR WIRE CUTTERS, ONCE A POPULAR TREATMENT, IS NO LONGER RECOMMENDED DUE TO THE EASE WITH WHICH THE INCISORS CAN FRACTURE (BREAK), RESULTING IN PAIN AND INFECTION. YOU MAY WISH TO DISCUSS WITH YOUR VETERINARIAN THE OPTION OF HAVING CERTAIN PROBLEM TEETH REMOVED UNDER GENERAL ANESTHETIC.
“CLIPPING THE TEETH WITH NAIL TRIMMERS OR WIRE CUTTERS, ONCE A POPULAR TREATMENT, IS NO LONGER RECOMMENDED DUE TO THE EASE WITH WHICH THE INCISORS CAN FRACTURE (BREAK), RESULTING IN PAIN AND INFECTION.”
UTERINE ADENOCARCINOMA IS TREATED SURGICALLY BY SPAYING THE RABBIT. BECAUSE THE COST OF THE PROCEDURE IS HIGHER WHEN THE RABBIT IS SICK (RABBITS WITH UTERINE CANCER MAY NEED INTENSIVE CARE SUCH AS HOSPITALIZATION, FLUID THERAPY, AND FORCE-FEEDING), EARLY SPAYING TO PREVENT THE PROBLEM IS RECOMMENDED. UTERINE INFECTIONS MAY ALSO REQUIRE SPAYING IN ADDITION TO ANTIBIOTICS.
TREATMENT OF SORE HOCKS CAN BE DIFFICULT AND CHALLENGING, ESPECIALLY IN THE LATER STAGES OF THE CONDITION. TREATMENT REQUIRES ANTIBACTERIAL MEDICATIONS TO CONTROL THE INFECTION, COUPLED WITH CLEANING OF THE SORES ON THE HOCKS. PROVIDING SOFT BEDDING IS ESSENTIAL TO ALLOW THE SORES TO HEAL. WHEN CAUGHT EARLY, THE HOCKS CAN USUALLY BE TREATED WITHOUT MUCH EFFORT. HOWEVER, THIS CAN EASILY BECOME A CHRONIC, STUBBORN, DEEP INFECTION.
THIS CLIENT INFORMATION SHEET IS BASED ON MATERIAL
WRITTEN BY: RICK AXELSON, DVM
ARE YOU PROVIDING YOUR PET RABBIT WITH THE PROPER BASIC CARE?
HEAD-SHAKING AND HEAD-TILTING MAY BE A SIGN OF THIS INFECTION.
DO YOU KNOW THE MOST COMMON HEALTH PROBLEMS IN DOGS?
FIND OUT WHY AND READ MORE SUMMER PET-SAFETY TIPS HERE.
PREVENTING HEAT STRESS AND INJURY IN PETS
BY DR. DENNIS CHEW | AUGUST 12, 2012
IT ALWAYS AMAZES ME WHEN, EVERY YEAR AS THE TEMPERATURES RISE, THERE ARE STILL REPORTS OF ANIMALS BEING LEFT ALONE INSIDE HOT VEHICLES, DESPITE THE FACT THAT THE DANGERS OF DOING SO ARE WELL-KNOWN. ANIMALS THAT EXERCISE TOO VIGOROUSLY IN THE HEAT OR CANNOT SEEK RELIEF FROM IT ARE ALSO AT RISK FOR ILLNESS AND INJURY AS WELL. NOT TOO LONG AGO, I HAD A CONCERNING EXPERIENCE LIKE THIS WITH MY OWN DOG WHEN I TOOK HIM OUT FOR A LITTLE FUN IN THE DOG PARK.THAT’S WHY, AS THE DOG DAYS OF SUMMER ARRIVE, I THOUGHT IT MIGHT BE HELPFUL TO REVIEW SOME SIMPLE FACTS ABOUT HOW THE HEAT CAN AFFECT OUR PETS.
BALMY WEATHER? STILL DEADLY
IT’S IMPORTANT TO REALIZE THAT DOGS AND CATS CAN DEVELOP HEAT-RELATED INJURY QUICKLY WHEN THEY STAY INSIDE A PARKED CAR OR OTHER VEHICLE. THIS CAN HAPPEN EVEN WHEN THE WINDOWS ARE PARTIALLY LOWERED, THE VEHICLE IS IN THE SHADE, OR THE OUTSIDE TEMPERATURES SEEM RELATIVELY MODERATE. MANY PEOPLE DO NOT REALIZE JUST HOW QUICKLY THE INTERIOR TEMPERATURE OF A CAR CAN INCREASE TO DEADLY LEVELS, EVEN WITH SOME AIRFLOW PROVIDED BY CRACKED WINDOWS. FOR EXAMPLE, ON A 90-DEGREE DAY, THE TEMPERATURE INSIDE A CLOSED CAR CAN CLIMB TO 109 DEGREES WITHIN JUST 10 MINUTES. IN LESS THAN 50 MINUTES, TEMPERATURES IN THAT SAME CAR CAN RISE TO ABOVE 130 DEGREES. ON EVEN A COMPARATIVELY BALMY 70-DEGREE DAY, TEMPERATURES INSIDE A VEHICLE CAN REACH TRIPLE DIGITS WITHIN 30 MINUTES (SEE TABLE).
HEAT TOXICITY CAN ALSO OCCUR IN DOGS THAT EXERCISE TOO VIGOROUSLY DURING PERIODS OF HIGH HEAT, ESPECIALLY IF THE HUMIDITY IS ALSO ELEVATED. EVEN DOGS THAT ARE IN GOOD ATHLETIC SHAPE AND USED TO REGULAR EXERCISE CAN DEVELOP HEAT INJURY WHEN OUT AND ABOUT IN EXTREME CONDITIONS. HEAT TOXICITY, OR HEAT INJURY, CAN RUN THE GAMUT FROM HEAT EXHAUSTION (WHICH OCCURS IN THE EARLY STAGES OF A HEAT-RELATED EVENT) TO HEAT STROKE, WHICH IS A FULL-BLOWN EMERGENCY THAT REQUIRES IMMEDIATE VETERINARY INTERVENTION.
THIS CHART WAS ORIGINALLY PUBLISHED IN THE JOURNAL PEDIATRICS. IT ALSO APPEARS ON THE AMERICAN VETERINARY MEDICAL ASSOCIATION SITE PAGE ABOUT PET SAFETY IN CARS. TO BETTER UNDERSTAND THE FACTORS THAT CAN CAUSE A CAR’S INTERIOR TEMPERATURE TO SKYROCKET EVEN WHEN IT IS COOL OUTSIDE, READ THIS ARTICLE BY JAN NULL, CCM.
WHAT HAPPENS TO A HEAT-STRESSED PET?
DURING HEAT STRESS, THE ANIMAL’S INTERNAL BODY TEMPERATURE CAN INCREASE RAPIDLY, AND FATAL ORGAN FAILURE CAN FOLLOW. SINCE DOGS AND CATS DO NOT SWEAT (EXCEPT ON FOOTPADS AND THE NOSE) THE WAY HUMANS DO, THEY CANNOT USE THIS AS A METHOD TO LOWER BODY TEMPERATURE. INSTEAD, DOGS AND CATS TRY TO REGULATE THEIR BODY TEMPERATURE BY PANTING TO HELP BODY HEAT DISSIPATE. THIS RESPONSE, HOWEVER, IS LIMITED AND EASILY OVERWHELMED UNDER EXTREME CONDITIONS.
SIGNS OF HEAT STRESS
INITIAL SIGNS OF HEAT TOXICITY INCLUDE:
- PANTING
- EXCESSIVE SALIVATION (WHICH IS OFTEN THICK AND ROPEY)
- WEAKNESS
- COLLAPSE
- BRIGHT RED MEMBRANES OF THE MOUTH, TONGUE, EYES, AND SOMETIMES SKIN IN LIGHT-PIGMENTED DOGS
- VOMITING AND DIARRHEA CAN ALSO OCCUR DUE TO DAMAGE TO THE GASTROINTESTINAL TRACT
MULTIPLE ORGANS CAN FAIL IF THE EXCESSIVE HEAT RETENTION IS NOT RELIEVED SOON ENOUGH. THESE ORGANS INCLUDE THE GASTROINTESTINAL TRACT, KIDNEYS, LIVER, HEART, MUSCLES, BRAIN, AND BONE MARROW. HEAT RETENTION CAUSES THE BLOOD VESSELS TO DILATE, AND A FORM OF SHOCK DEVELOPS AS THE CONDITION ADVANCES.
IF THE ANIMAL IS IN A STATE OF COLLAPSE WHEN FOUND, IT IS IMPERATIVE TO GET HIM TO YOUR LOCAL VETERINARIAN OR AN EMERGENCY CLINIC IMMEDIATELY. QUICKLY COOLING THE ANIMAL FOR THE TRIP WITH COOL WATER FROM A GARDEN HOSE MAY BE HELPFUL BUT DO NOT IMMERSE YOUR DOG IN COLD OR ICE WATER AS THIS COULD LEAD TO SHOCK. IF SHOCK DOES DEVELOP, INTRAVENOUS FLUIDS AND OTHER MEDICATIONS MAY BE NEEDED FOR A FEW DAYS UPON ARRIVAL AT THE HOSPITAL.
PREVENTING HEAT STRESS
NEVER ASSUME THAT IT IS OK TO LEAVE YOUR DOG OR CAT IN A CAR UNATTENDED DURING WARMER WEATHER, AND CAREFULLY MONITOR AND LIMIT STRENUOUS EXERCISE PERIODS FOR YOUR DOG IN HIGH TEMPERATURES. REDUCE THE TIME YOU ALLOW YOUR DOG TO WALK, RUN OR JOG WITH YOU, OR TO FOLLOW YOU DURING BIKE RIDES. IF IT’S HOT ENOUGH, YOU MAY NEED TO POSTPONE THE ACTIVITY ALTOGETHER. KEEP IN MIND THAT OBESE DOGS OR ONES THAT ONLY EXERCISE OCCASIONALLY ARE PARTICULARLY VULNERABLE TO OVERHEATING.
EVEN ON A REDUCED EXERCISE SCHEDULE, TAKE FREQUENT REST BREAKS IN THE SHADE. REMEMBER TO TAKE WATER AND EVEN ICE CUBES ALONG FOR YOUR DOG TO DRINK WHEN OUTDOOR TEMPERATURES ARE ABOVE 80 DEGREES. TOWELS THAT CAN BE WET WITH COOL WATER AND PLACED OVER YOUR DOG CAN HELP BRING HIS BODY TEMPERATURE DOWN FOLLOWING EXERCISE BOUTS — BUT BE SURE TO REMOVE THE TOWELS ONCE THEY BECOME WARMED FROM BODY HEAT. EXERCISING IN DOG PARKS EARLY IN THE MORNING OR LATER AT NIGHT WHEN OUTSIDE TEMPERATURES ARE LOWER WILL ALSO REDUCE THE RISK FOR HEAT-RELATED INJURY. RESTRICT EXERCISE WHEN OUTSIDE TEMPERATURES ARE ABOVE 80 DEGREES, ESPECIALLY IN LOCALES WITH HIGH HUMIDITY. FINALLY, DOGS WITH LONG HAIR MAY BENEFIT FROM BEING CLIPPED OR SHAVED FOR THE SUMMER MONTHS.
MY OWN PERSONAL EXPERIENCE
RECENTLY, MY OWN DOG WAS VIGOROUSLY EXERCISING IN THE DOG PARK — RUNNING AROUND WITH TWO OTHER DOGS AND HAVING A GREAT TIME. THE AMBIENT TEMPERATURE WAS ABOUT 92 DEGREES, AND THE HUMIDITY WAS QUITE HIGH. HE WAS FINE FOR ABOUT FIVE MINUTES, BUT THEN STARTED TO SALIVATE A LOT AND WAS PANTING VERY RAPIDLY. WE REMOVED HIM FROM THE PARK AND WALKED BACK TO THE CAR. HE COULD NOT JUMP INTO THE CAR ON HIS OWN, AND I HAD TO LIFT HIM INTO THE VEHICLE. HE WAS EXTREMELY QUIET AND DIDN’T MOVE DURING THE FIVE-MINUTE DRIVE HOME. I KEPT THE AIR-CONDITIONING ON HIGH WITH THE VENTS DIRECTED HIS WAY. UPON ARRIVAL AT THE HOUSE, I HOSED HIM DOWN FOR FIVE MINUTES WITH COOL WATER FROM THE GARDEN HOSE. HE REVIVED OVER THE NEXT 10 MINUTES. HAD HE NOT COME AROUND RIGHT AWAY, WE WOULD HAVE BEEN ON OUR WAY TO THE EMERGENCY CLINIC FOR IV FLUIDS. THIS INCIDENT UNDERSCORED FOR ME JUST HOW EASY IT IS FOR A DOG TO GET INTO TROUBLE IN THE HEAT — EVEN WITH A WATCHFUL VETERINARIAN AS AN OWNER. IF YOU SEE ANY POTENTIAL SIGNS OF DISTRESS IN YOUR DOG, BE SURE TO TAKE PROMPT STEPS TO COOL HIM. AND IF YOU HAVE ANY DOUBT ABOUT HOW SERIOUS THE SITUATION MAY OR MAY NOT BE, CALL YOUR VETERINARIAN IMMEDIATELY.
WELLNESS IN GERIATRIC DOGS
WHAT IS WELLNESS TESTING?
WELLNESS TESTING IS THE TERM GIVEN TO A GROUP OF TESTS THAT IS PERFORMED SPECIFICALLY TO DETECT SIGNS OF EARLY OR SUBCLINICAL DISEASE IN A PET THAT IS APPARENTLY HEALTHY.
WHY DO WELLNESS TESTING?
“…STEPS CAN OFTEN BE TAKEN TO MANAGE OR CORRECT THE PROBLEM BEFORE IRREVERSIBLE DAMAGE OCCURS.”
PETS CANNOT TELL YOU HOW THEY ARE FEELING, AND AS A RESULT, DISEASE MAY BE PRESENT BEFORE YOU ARE AWARE OF IT. IF A DISEASE OR CONDITION CAN BE DETECTED BEFORE A PET SHOWS SIGNS OF ILLNESS, STEPS CAN OFTEN BE TAKEN TO MANAGE OR CORRECT THE PROBLEM BEFORE IRREVERSIBLE DAMAGE OCCURS. WELLNESS TESTING IS PARTICULARLY IMPORTANT IN THE GERIATRIC PET, SINCE THERE IS A GREATER CHANCE THAT UNDERLYING DISEASE MAY BE PRESENT.
WHEN IS WELLNESS TESTING DONE?
WELLNESS TESTING SHOULD BE DONE ON A REGULAR BASIS, AND MANY PET OWNERS COMBINE WELLNESS TESTING WITH THEIR ANNUAL VISIT TO THE VETERINARIAN FOR THEIR DOG’S PHYSICAL EXAMINATION, VACCINATION, AND HEARTWORM TESTING. YOUR VETERINARIAN MAY RECOMMEND MORE FREQUENT TESTING DEPENDING ON YOUR DOG’S AGE OR SPECIFIC HEALTH CONCERNS. MONITORING YOUR PET’S HEALTH STATUS ON A REGULAR BASIS MAKES IT EASIER FOR THE VETERINARIAN TO DETECT MINOR CHANGES THAT SIGNAL THE ONSET OF DISEASE.
WHAT IS INVOLVED IN WELLNESS TESTING?
THERE ARE FOUR MAIN CATEGORIES OF WELLNESS TESTING FOR THE GERIATRIC DOG: COMPLETE BLOOD COUNT (CBC), BIOCHEMISTRY PROFILE, URINALYSIS, AND THYROID HORMONE TESTING. WITHIN EACH CATEGORY, YOUR VETERINARIAN WILL ADVISE YOU ABOUT HOW EXTENSIVE THE TESTING SHOULD BE. IN YOUNGER DOGS WITHOUT NOTICEABLE HEALTH COMPLAINTS, RELATIVELY SIMPLE TESTING MAY BE ADEQUATE. HOWEVER, IN THE GERIATRIC DOG, MORE COMPREHENSIVE TESTING IS RECOMMENDED.
THIS SIMPLE BLOOD TEST ANALYSES THE CELLULAR COMPONENTS IN THE BLOODSTREAM. THESE INCLUDE RED BLOOD CELLS, WHICH CARRY OXYGEN TO THE TISSUES, WHITE BLOOD CELLS, WHICH FIGHT INFECTION AND RESPOND TO INFLAMMATION, AND PLATELETS, WHICH HELP THE BLOOD TO CLOT. THE CBC PROVIDES DETAILS ABOUT THE NUMBER, SIZE, AND SHAPE OF THE VARIOUS CELLS TYPES, AND IDENTIFIES THE PRESENCE OF ANY ABNORMAL CELLS. (SEE HANDOUT COMPLETE BLOOD COUNT).
BIOCHEMISTRY PROFILE –
THIS IS A SERIES OF TESTS PERFORMED ON SERUM, WHICH IS THE LIQUID COMPONENT OF BLOOD. THESE TESTS PROVIDE INFORMATION ABOUT HOW WELL THE VARIOUS ORGANS OF THE BODY ARE WORKING, AND HELP TO DETECT THE PRESENCE OF SOME METABOLIC DISEASES. THERE ARE TESTS TO ASSESS THE LIVER AND KIDNEYS, TESTS TO IDENTIFY THE PRESENCE OF DIABETES, AND SO ON. (SEE HANDOUT SERUM BIOCHEMISTRY).
“IN SOME CASES, A MORE EXTENSIVE DIAGNOSTIC WORKUP MAY BE RECOMMENDED…”
IF MINOR ABNORMALITIES ARE FOUND ON THE BIOCHEMISTRY PROFILE, THE VETERINARIAN MAY SIMPLY REQUEST THAT YOU REPEAT THE TESTS AT A LATER TIME; DEPENDING ON THE ABNORMALITY, THIS MAY BE IN A FEW DAYS, A FEW WEEKS, OR A FEW MONTHS. IN SOME CASES, A MORE EXTENSIVE DIAGNOSTIC WORKUP MAY BE RECOMMENDED, INCLUDING AN EXPANDED BIOCHEMISTRY PROFILE, OR SPECIAL TESTS AND/OR IMAGING (X-RAYS, ULTRASOUND).
URINE EVALUATION INCLUDES AN ANALYSIS OF THE CHEMICAL COMPONENTS IN THE SAMPLE, AS WELL AS A MICROSCOPIC EXAMINATION OF THE CELLS AND SOLID MATERIAL THAT MAY BE PRESENT (SEE OUR HANDOUT “URINALYSIS”). URINALYSIS PROVIDES INFORMATION ABOUT HOW WELL THE KIDNEYS ARE WORKING, IDENTIFIES THE PRESENCE OF INFLAMMATION OR INFECTION IN THE KIDNEYS AND URINARY SYSTEM, AND MAY DETECT THE PRESENCE OF UNDERLYING METABOLIC DISEASE SUCH AS DIABETES. URINALYSIS IS NECESSARY FOR A COMPLETE ASSESSMENT OF THE URINARY SYSTEM. IT SHOULD BE PERFORMED ROUTINELY AS PART OF WELLNESS TESTING, AND IS PARTICULARLY IMPORTANT IN THE GERIATRICwellness_dog_geriatric-4DOG BECAUSE OF THE INCREASED RATE OF KIDNEY DISEASE IN THE OLDER PET.
THE THYROID GLAND IS LIKE A “THERMOSTAT”, WHICH “SETS” THE METABOLIC RATE OF THE WHOLE BODY (SEE HANDOUT THYROID TESTING). THE MOST COMMON THYROID DISEASE IN THE DOG ISHYPOTHYROIDISM, WHICH OCCURS WHEN THE THYROID GLAND DOES NOT PRODUCE ENOUGH THYROID HORMONE. THE FUNCTION OF THE THYROID GLAND SHOULD BE TESTED ROUTINELY IN OLDER DOGS, ESPECIALLY IF THERE IS UNEXPLAINED WEIGHT GAIN, LACK OF ENERGY, RECURRING SKIN OR EAR INFECTIONS, OR HAIR LOSS ON THE BODY AND TAIL,
SUMMARY
WELLNESS TESTING IS A SIMPLE AND EFFECTIVE WAY OF MONITORING YOUR OLDER DOG’S HEALTH. EARLY DETECTION AND CORRECTION OF MEDICAL PROBLEMS HELP TO ENSURE THAT YOUR PET WILL BE HEALTHY AND ACTIVE FOR AS LONG AS POSSIBLE.
THIS CLIENT INFORMATION SHEET IS BASED ON MATERIAL
WRITTEN BY: KRISTIINA RUOTSALO, DVM, DVSC, DIP ACVP & MARGO S. TANT BSC, DVM, DVSC
ACHES AND PAINS? MAYBE IT’S ARTHRITIS.
DID YOU KNOW A CAT CAN SPRINT UP TO 30 MILES AN HOUR?
IS YOUR PET DRINKING WATER EXCESSIVELY? IT COULD BE A SIGN OF THIS DISEASE.
ADDISON’S DISEASE IN DOGS – OVERVIEW
WHAT IS ADDISON’S DISEASE?
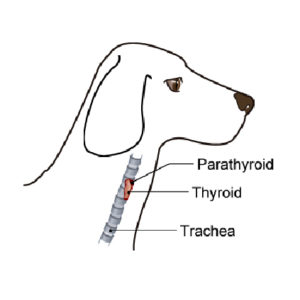
ADDISON’S DISEASE IS THE COMMON NAME FOR HYPOADRENOCORTICISM, CAUSED BY DECREASED HORMONE PRODUCTION FROM THE OUTER PART OR CORTEX OF THE ADRENAL GLAND.
WHAT ARE THE ADRENAL GLANDS AND WHAT DO THEY DO?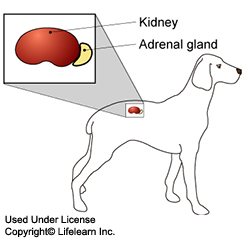 THE ADRENAL GLANDS ARE SMALL, PAIRED GLANDS LOCATED NEAR THE KIDNEYS. EACH GLAND CONSISTS OF AN OUTER CORTEX AND AN INNER MEDULLA. THE GLANDS PRODUCE TWO IMPORTANT HORMONES THAT REGULATE A VARIETY OF BODY FUNCTIONS AND ARE NECESSARY TO SUSTAIN LIFE. THE TWO HORMONES ARE CORTISOL, A STRESS HORMONE, AND ALDOSTERONE, A HORMONE THAT REGULATES THE BODY’S LEVELS OF THE MINERALS SODIUM AND POTASSIUM. SODIUM AND POTASSIUM LEVELS ARE IMPORTANT FOR MAINTAINING THE BODY’S FLUID BALANCE.
THE ADRENAL GLANDS ARE SMALL, PAIRED GLANDS LOCATED NEAR THE KIDNEYS. EACH GLAND CONSISTS OF AN OUTER CORTEX AND AN INNER MEDULLA. THE GLANDS PRODUCE TWO IMPORTANT HORMONES THAT REGULATE A VARIETY OF BODY FUNCTIONS AND ARE NECESSARY TO SUSTAIN LIFE. THE TWO HORMONES ARE CORTISOL, A STRESS HORMONE, AND ALDOSTERONE, A HORMONE THAT REGULATES THE BODY’S LEVELS OF THE MINERALS SODIUM AND POTASSIUM. SODIUM AND POTASSIUM LEVELS ARE IMPORTANT FOR MAINTAINING THE BODY’S FLUID BALANCE.
WHAT CAUSES ADDISON’S DISEASE?
ADDISON’S DISEASE IN THE DOG IS PRIMARILY CAUSED BY AN IMMUNE –MEDIATED DESTRUCTION OF ADRENAL TISSUE. LESS COMMONLY, THE ADRENAL GLANDS MAY BE DAMAGED BY TRAUMA OR INFECTION. ADDISON’S DISEASE CAN ALSO OCCUR FOLLOWING TREATMENT OF CUSHING’S DISEASE (HYPERADRENOCORTICISM), IN WHICH TOO MUCH CORTISOL AND ALDOSTERONE ARE PRODUCED. IF THE MEDICATION USED TO TREAT CUSHING’S DISEASE INADVERTENTLY SUPPRESSES TOO MUCH ADRENAL GLAND ACTIVITY, DEFICIENCY OF CORTISOL AND ALDOSTERONE MAY RESULT.
A SECONDARY FORM OF ADDISON’S DISEASE CAN RESULT FROM A TUMOR OR DEFECT IN THE PITUITARY GLAND, WHICH IS AN IMPORTANT HORMONAL REGULATOR LOCATED IN THE BRAIN. SECONDARY ADDISON’S DISEASE CAN ALSO DEVELOP IF A DOG HAS BEEN TREATED WITH LONG-TERM STEROIDS FOR ANY REASON AND THE MEDICATION IS ABRUPTLY STOPPED. THIS LAST CONDITION IS KNOWN AS IATROGENIC HYPOADRENOCORTICISM AND IS GENERALLY TEMPORARY.
CERTAIN BREEDS SEEM TO BE AT INCREASED RISK FOR DEVELOPING ADDISON’S DISEASE. THESE INCLUDE, BUT ARE NOT LIMITED TO: PORTUGUESE WATER DOG, BEARDED COLLIE, STANDARD POODLES, NOVA SCOTIA DUCK TOLLING RETRIEVERS, LEONBERGERS, AND LABRADOR RETRIEVERS.
WHAT ARE THE CLINICAL SIGNS OF HYPOADRENOCORTICISM?
“CLINICAL SIGNS OF ADDISON’S DISEASE ARE USUALLY VAGUE AND NON-SPECIFIC.”
CLINICAL SIGNS OF ADDISON’S DISEASE ARE USUALLY VAGUE AND NON-SPECIFIC. ADDISONIAN PATIENTS MAY PRESENT WITH LETHARGY, DIARRHEA, VOMITING, INCREASED THIRST, INCREASED URINATION, AND UNPLANNED WEIGHT LOSS. INTERMITTENT SHAKING EPISODES ARE SOMETIMES SEEN. THE SYMPTOMS MAY WAX AND WANE.
NON-SPECIFIC MEDICAL TREATMENT LIKE THE ADMINISTRATION OF FLUIDS OR CORTICOSTEROIDS APPEARS TO HELP TEMPORARILY, BUT THE SIGNS SOON RETURN. IF A PET EXPERIENCES RECURRENT BOUTS OF SUDDEN LETHARGY, DIARRHEA AND VOMITING, INCREASED THIRST AND URINATION OR OTHER NON-SPECIFIC ILLNESS, ADDISON’S DISEASE SHOULD BE CONSIDERED AS AN UNDERLYING CAUSE.
WHAT IS AN ADDISONIAN CRISIS?
SOMETIMES THIS CONDITION TAKES ON A MUCH MORE SERIOUS PRESENTATION RESULTING IN SUDDEN WEAKNESS, WITH SEVERE VOMITING AND DIARRHEA, AND SOMETIMES COLLAPSE. THIS IS AN ADDISONIAN CRISIS AND IS CONSIDERED A MEDICAL EMERGENCY. IMMEDIATE HOSPITALIZATION AND SUPPORTIVE TREATMENT ARE NEEDED.
HOW IS ADDISON’S DISEASE DIAGNOSED?
DIAGNOSIS IS BASED ON YOUR PET’S MEDICAL HISTORY, INCLUDING ANY MEDICATIONS, CLINICAL SIGNS, AND THE RESULTS OF COMMON BLOOD AND URINE TESTS, MOST NOTABLY ELECTROLYTE IMBALANCES. THE MOST DEFINITIVE DIAGNOSTIC TEST FOR ADDISON’S DISEASE IS THE ACTH-STIMULATION TEST. IN THIS TEST, CORTISOL LEVELS ARE MEASURED BEFORE AND AFTER INJECTION OF A SYNTHETIC FORM OF ACTH. ADDITIONAL TESTS SUCH AS BASAL CORTISOL LEVELS, ENDOGENOUS PLASMA ACTH, ECG, RADIOGRAPHS OR ABDOMINAL ULTRASOUND MAY BE PERFORMED TO RULE-OUT ANOTHER CAUSE FOR YOUR PET’S CLINICAL SIGNS. IN RARE INSTANCES MRI OR CT MAY BE NEEDED TO DIAGNOSE A PITUITARY GLAND PROBLEM.
HOW IS ADDISON’S DISEASE TREATED? ONCE DIAGNOSED, MOST DOGS WITH ADDISON’S DISEASE CAN BE SUCCESSFULLY TREATED.
ONCE DIAGNOSED, MOST DOGS WITH ADDISON’S DISEASE CAN BE SUCCESSFULLY TREATED.
PERCORTEN®-V (DESOXYCORTICOSTERONE PIVALATE – DOCP) IS AN INJECTABLE MEDICATION APPROVED BY THE FDA FOR TREATMENT OF ADDISON’S DISEASE IN DOGS. IT IS INJECTED EVERY 3 – 4 WEEKS, DEPENDING ON THE PATIENT, AND REPLACES THE MISSING MINERALOCORTICOID ALDOSTERONE. IT IS SUPPLEMENTED BY AN ORAL GLUCOCORTICOID. WITH A LITTLE TRAINING, DOCP INJECTIONS CAN BE GIVEN AT HOME.
DOCP IS NOT FOR EVERY DOG, AND SOME ADDISON’S PATIENTS DO BEST ON ORAL MEDICATIONS THAT REPLACE BOTH THE MINERALOCORTICOID AND THE GLUCOCORTICOID.
YOUR DOG’S DIET AND ACTIVITY LEVELS CAN OFTEN REMAIN UNCHANGED. THE MAJORITY OF DOGS RESUME NORMAL LIVES, EVEN AFTER AN ADDISONIAN CRISIS. YOUR VETERINARIAN WILL DISCUSS ADDISON’S TREATMENT OPTIONS WITH YOU AND DECIDE WHICH THERAPY IS BEST FOR YOUR DOG.
WHAT IS THE PROGNOSIS FOR A DOG DIAGNOSED WITH ADDISON’S DISEASE?
THE VAST MAJORITY OF PATIENTS WITH ADDISON’S DISEASE HAVE A GOOD TO EXCELLENT PROGNOSIS ONCE THE DIAGNOSIS IS MADE AND THEY HAVE BEEN STABILIZED WITH THE APPROPRIATE MEDICATIONS. IF YOU WISH TO DISCUSS THE LONG-TERM PROGNOSIS FOR YOUR PET, PLEASE DO NOT HESITATE TO CONTACT YOUR VETERINARIAN.
THIS CLIENT INFORMATION SHEET IS BASED ON MATERIAL
WRITTEN BY: ERNEST WARD, DVM & ROBIN DOWNING, DVM, CVPP, CCRP, DAAPM.
DO YOU KNOW HOW IMPORTANT THIS VACCINATION IS?
THIS VACCINE CAN HELP PREVENT ONE OF THE MOST SERIOUS INFECTIOUS DISEASES IN CATS.
SOCIALIZING YOUR PUPPY IS CRUCIAL TO MINIMIZING FEARS IN ADULTHOOD. FIND OUT WHAT YOU CAN DO HERE.
CPR CAN SAVE THE LIVES OF ANIMALS, TOO!
UNDERSTAND WHY DOGS BITE AND HOW TO AVOID ATTACKS.
EDUCATE CHILDREN ON HOW TO PROPERLY INTERACT WITH DOGS.
IT’S NATIONAL DOG BITE PREVENTION WEEK. LEARN HOW TO PROPERLY INTRODUCE YOURSELF TO A DOG.
SKIN FOLD DERMATITIS
FEBRUARY 27, 2014
Wrinkly dogs like Pugs are so cute. What’s not so cute? The skin disease that can result from improper care of the skin in those wrinkles. Skin fold dermatitis, which can also happen to catswith squished faces, is caused by the warm, moist conditions that can occur in deep skin folds on the face, at the tail, or around the private parts of females. It causes hair loss, skin irritation, and a bad smell in those folds, and leads to a skin infection called pyoderma. Treatment involves cleaning the affected areas thoroughly and applying or administeringantimicrobials. In severe cases, a veterinarian might want to surgically remove the excess skin folds.
Overview
Skin fold dermatitis is a skin condition most common in breeds with pronounced facial, tail, and vulvar folds, in particular, though any deep skin fold anywhere in the body can be susceptible to skin fold dermatitis.
This condition occurs when skin folds are deep, causing abnormal rubbing and retaining moisture in an area that’s both warm and not well aerated. These conditions are ideal for the overgrowth of normal skin inhabitants like yeast and bacteria. The resulting skin inflammation, called dermatitis, typically leads to a skin infection called pyoderma. Chronic pyoderma is typical in cases of skin fold dermatitis.
Though not a genetic disease, per se, skin characteristics that include wrinkles and deep skin folds are more common in certain breeds. In pets already predisposed to skin fold dermatitis, obesity can exacerbate the condition. Underlying skin disease (such as allergic skin disease) will also aggravate the condition, often severely.
Signs and Identification
Skin fold dermatitis is easily identified as typically hairless (alopecic), reddened, and malodorous areas of folded skin or creases/wrinkles. In the case of deep facial folds (typical of brachycephalic dogs and cats), brown staining of facial fur (secondary to components in tears) can make these folds look more pronounced.
Tail fold dermatitis (typical to dogs with corkscrew tails), when especially severe, can lead to deep, severe infections. These deep tail folds are typically identified by probing the tail base with a cotton-tipped swab to determine its depth.
Vulvar tail fold dermatitis can occur in female dogs that have excess skin folds around their private area. Urinary tract infection can occur as a consequence of vulvar skin fold pyoderma.
Affected Breeds
All brachycephalic (short-headed, flat-nosed) breeds that have facial folds are similarly predisposed to skin fold dermatitis of this area (Bulldogs, Pugs, Shih Tzus, etc). “Wrinkly” dogs like Shar-Peis and Bloodhoundsare also affected. Likewise, dogs with corkscrew tails (English Bulldogs, for example) can be affected.
Cats that have facial folds (Persians, for example) or are overweight (creating more skin folds) are also at risk.
Treatment
Treatment for skin fold dermatitis involves cleaning of the affected areas and frequent use of topical or systemic (oral or injectable) antimicrobial medications to manage the resulting pyodermas.
Surgical intervention may be recommended for moderate to severely affected animals. Removing the abnormal skin folds will, in many cases, yield a complete cure.
Treating any underlying skin disease and maintaining a healthy body weight can reduce the severity or even eliminate skin fold dermatitis.
Prevention
To help keep your pet free of skin fold dermatitis, watch your pet’s weight, and carefully clean the skin folds regularly; be sure to used products that are approved for pets and (if facial folds are present) are safe to use around the eyes and face. Also, work with your vet on treating any skin conditions.
This article has been reviewed by a Veterinarian.
IS YOUR DOG CONSTANTLY LICKING HIS PAWS? IT COULD BE ALLERGIES.
ITCHY CAT? THIS SURPRISING SOURCE COULD BE THE CULPRIT.
THESE TIPS FOR YOUR CAT CAN HELP PREVENT CANCER.
WHAT CAN WE LEARN FROM 3,000 GOLDEN RETRIEVERS? FIND OUT HERE!
FOUND A LUMP ON YOUR DOG? NOW WHAT?
HAVE QUESTIONS ABOUT CANCER IN DOGS? GET ANSWERS HERE.
NATIONAL HAIRBALL AWARENESS DAY
Posted by Karen on April 24, 2015
Today is National Hairball Awareness Day, a special day to highlight causes, treatments and prevention of hairballs.
The occurrence of hairballs was simple to explain when cats primarily lived outdoors: Their shedding cycle was determined by natural cycles of light that occur in nature. They shed their thicker winter coats in spring in exchange for a thinner summer coat. The situation reversed itself once the weather turned colder, and hours of light diminished.
Indoor cat’s bodies are thrown off by living indoors where lights are on at hours that don’t coincide with Mother Nature.
Other reasons a cat’s body is thrown off its natural coat shedding rhythms include temperature, nutrition, hormones, body chemicals, genetics and the health of the cat.
Hairballs are balls of hair that form in a cat’s stomach as a result of grooming. While any cat can develop a hairball, they tend to be more prevalent in long-haired cats. Hairballs are ejected from the stomach in long, moist tubes called trichobezoars. While it’s normal for cats to have hairballs on occasion, it isn’t normal to have them multiple times a week.
Hairballs are more than an annoyance for pet parents, they can cause serious health issues requiring veterinary care such as:
- Ongoing vomiting, gagging, retching or hacking without producing a hairball
- Lack of appetite
- Lethargy
- Constipation (intestinal blockage may have taken place)
- Diarrhea
- Bloated abdomen:
Here are some ways to prevent hairballs from forming
- Brush your cat daily or at minimum several times a week
- Make sure your cat has enough moisture in his/her diet. If your cat’s diet consists solely of dry kibble, consider adding canned food to his diet.
- Add a little fiber to your cat’s diet. A teaspoonful of pure pumpkin puree daily will help reduce hairballs, and allow ones that form to be eliminated easier
- Add an omega-3 supplement (krill oil is a good choice).
- Is your cat grooming constantly? Some cats groom constantly as a way to combat boredom. Try scheduling more play sessions with your cat or present a new toy to distract him from compulsively grooming
Watch for changes in your cat’s behavior because cats are experts at covering up health issues. If you notice any changes in your cat’s behavior, such as eating, litter box usage, or energy level, consult your veterinarian right away.
Written by Karen
Karen is Publisher of Fully Feline. She also owns a pet care business in Overland Park, KS called Joy of Living.
German Shepherds, St. Bernards, and Labrador Retrievers can be predisposed to this condition.
Emotions and tone — do our pets understand more than we think?
Does your cat make the most dog-like list?
What’s in your pet’s food? Learn the label!
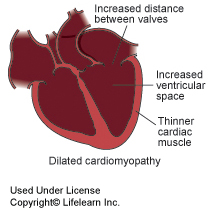
What is cardiomyopathy?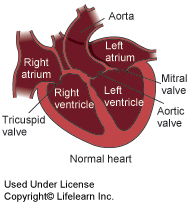 Cardiomyopathy is a term used to describe diseases of the heart muscle. In cats, three classes of cardiomyopathy have been described: hypertrophic, dilated, and intermediate or restrictive cardiomyopathy. In all classes, the heart disease usually results in clinical signs of heart failure. Cardiomyopathy may be seen as a primary condition or secondary to other diseases.
Cardiomyopathy is a term used to describe diseases of the heart muscle. In cats, three classes of cardiomyopathy have been described: hypertrophic, dilated, and intermediate or restrictive cardiomyopathy. In all classes, the heart disease usually results in clinical signs of heart failure. Cardiomyopathy may be seen as a primary condition or secondary to other diseases.
What are the clinical signs seen with cardiomyopathy?
“Often cats will alter their activity levels to those that they can cope with, which make it difficult to diagnose cardiomyopathy until it is quite advanced.”
In the early stages of disease, the cat may not show any signs of disease. This is referred to as compensated heart disease. Often cats will alter their activity levels to those that they can cope with, which make it difficult to diagnose cardiomyopathy until it is quite advanced. In the long term, cats with any type of cardiomyopathy are at an increased risk of developing congestive heart failure, thromboembolic disease, and hypertension.
 Development of congestive heart failure – Breathlessness and lethargy are the most frequently noticed signs of congestive heart failure and result from failure of the heart to pump blood efficiently.
Development of congestive heart failure – Breathlessness and lethargy are the most frequently noticed signs of congestive heart failure and result from failure of the heart to pump blood efficiently.
Thromboembolic disease – Altered flow of blood in the enlarged heart chambers increases the risk of blood clot formation within the heart called a thrombus. If parts of the thrombus become dislodged, they can travel in the bloodstream and block smaller blood vessels. These travelling blood clots are called emboli and the most common place for them to lodge is at the bottom of the aorta, which is the largest artery in the body. This results in obstruction of the blood supply to the back legs, which is very painful and leads to paralysis. This blockage is commonly referred to as a saddle thrombus or saddle thrombosis. Although some cats may recover with appropriate treatment, this is a potentially fatal complication of any cardiomyopathy.
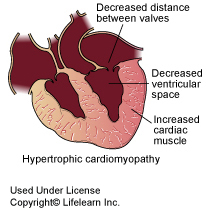 Hypertension – High blood pressure or hypertension is a possible complication seen in many cases of hypertrophic cardiomyopathy. This may result in spontaneous bleeding, such as nosebleeds or hemorrhage within the eye; it is a common cause of retinal detachment and sudden blindness in cats. This may be noticed as a sudden loss of vision and widely dilated pupils. The blindness will be permanent unless the retina is reattached within a couple of days, and requires immediate emergency treatment. Drugs that lower the blood pressure may be used to treat cats with this problem. Measuring blood pressure in cats is challenging due to their small size; in addition, blood pressure rises with stress, which makes interpretation of results difficult. In many cats, hypertension is detected only after a problem has occurred. Examination of the eyes may give early indications of hypertension since the blood vessels of the retina may show changes and small hemorrhages may be seen. For further information about hypertension, see our handout “Hypertension”.
Hypertension – High blood pressure or hypertension is a possible complication seen in many cases of hypertrophic cardiomyopathy. This may result in spontaneous bleeding, such as nosebleeds or hemorrhage within the eye; it is a common cause of retinal detachment and sudden blindness in cats. This may be noticed as a sudden loss of vision and widely dilated pupils. The blindness will be permanent unless the retina is reattached within a couple of days, and requires immediate emergency treatment. Drugs that lower the blood pressure may be used to treat cats with this problem. Measuring blood pressure in cats is challenging due to their small size; in addition, blood pressure rises with stress, which makes interpretation of results difficult. In many cats, hypertension is detected only after a problem has occurred. Examination of the eyes may give early indications of hypertension since the blood vessels of the retina may show changes and small hemorrhages may be seen. For further information about hypertension, see our handout “Hypertension”.
How is cardiomyopathy diagnosed?
Diagnosis of heart disease can be suspected based on clinical signs, chest x-rays, and electrocardiography (ECG). The specific diagnosis of the type of cardiomyopathy is made with a cardiac ultrasound or echocardiography.
In cases where hypertension is a possibility, blood pressure can be evaluated if suitable equipment is available. Retinal examination may provide evidence of hypertension where blood pressure measurements cannot be made.
Other tests, especially blood tests, may be done in order to check that the cardiomyopathy is not secondary to some other disease.
What causes cardiomyopathy?
Some cases of cardiomyopathy, especially restrictive cardiomyopathy, appear to be congenital. In older cats, hyperthyroidism commonly causes hypertrophic cardiomyopathy. Kidney failure may cause hypertension and cardiomyopathy. A previously common cause of dilated cardiomyopathy that is now rare is a dietary deficiency of taurine, which is an essential amino acid for the cat. Commercial cat food is supplemented with taurine, and this disease is only seen in cats that are fed imbalanced home-prepared diets or dog food.
How is cardiomyopathy treated?
“Hyperthyroidism is the most treatable cause of cardiomyopathy since complete resolution of the heart disease is possible if diagnosed and treated early.”
In cases where an underlying cause of the heart disease is found, then treatment of this condition may result in improvement or reversal of the heart disease. Hyperthyroidism is the most treatable cause of cardiomyopathy since complete resolution of the heart disease is possible if diagnosed and treated early. In cases where no cause is identified, called idiopathic cardiomyopathy, and in cases where the heart disease persists following treatment of the underlying cause then medication may be needed.
Treatment varies according to each case but may include:
1. Diuretics if congestive heart failure is present.
2. Beta-blockers to reduce the heart rate if it is excessive.
3. Calcium channel-blockers to help the heart muscle relax and hence help more effective filling of the heart.
4. Aspirin may be used for its effects at reducing the risk of thrombus formation and thromboembolic disease. Dosing of aspirin should always be as advised by a veterinarian since aspirin may be toxic to cats. Aspirin poisoning, which occurs if the dose or frequency of aspirin administration is too high, may cause vomiting and internal bleeding. If your cat shows these signs, stops eating or appears sick, aspirin therapy should be stopped and you should consult your veterinarian immediately.
5. Angiotensin Converting Enzyme (ACE) inhibitors – these drugs also help to control congestive heart failure.
6. Drugs to lower blood pressure – additional medications may be needed to treat hypertension.
What is the prognosis?
“Cats with idiopathic cardiomyopathy may remain stable for several years.”
The long-term prognosis for a cat with cardiomyopathy is extremely variable, depending on the cause of this disease. Cats with idiopathic cardiomyopathy may remain stable for several years.
Does a cat with cardiomyopathy need a special diet?
Cats with underlying kidney disease should be fed a special kidney diet to manage this disease. Depending on the clinical signs, your veterinarian may recommend a special heart diet instead of the kidney diet. Low sodium diets are often recommended for cats with idiopathic cardiomyopathy. This may decrease the risk of developing congestive heart failure and hypertension. Cat treats are often quite salty and should be avoided. Your veterinarian will make specific dietary recommendations, based on your pet’s condition.
This client information sheet is based on material written by: Ernest Ward, DVM
Do you know which medicines in your cabinet can be harmful?
Causes of feline paralysis
Being reunited with your lost pet: priceless.
This routine surgery could help prevent cancer.
Careful, your pet might find this deadly chemical tasty!
Spring holidays are around the corner – watch out for these Easter poisons.
Do you know the signs of kidney disease?
Common causes of bladder infections.
“Petting, scratching, cuddling a dog could be as soothing to the mind and heart as deep meditation, and almost as good for the soul as prayer.” – Dean Koontz
This life threatening condition requires emergency treatment.
Do you know the first signs of motion sickness in cats?
Have you heard of optic neuritis?
Saved by the stay: A few simple commands to make the world a safer place for your dog.
“I’m reflecting on the meowment.”
This new study suggests that your dog may be tuning in to what you say, not just how you say it.
A flavor too far: When medicines become too appealing to pets.
Even a tiny pet can display aggression. Learn the basics of bad bunny behavior.
Behavior issues can leave birds with no feathers to ruffle.
How many of these veterinary care basics do you know?
What to know when your dog needs a dental cleaning.
“If I could be half the person my dog is, I’d be twice the human I am.”—Charles Yu”
Learn more about high blood pressure in dogs.
Share your own picture of your beautiful senior dog.
Have the wintertime blues? Your pet might, too.
Choosing a toy for your parrot.
Did you know that e-cigarettes pose a nicotine poisoning risk to pets?
All about dry eye syndrome in dogs.
New year, new you, new Fluffy.
How important are vaccines to my dog’s health?
Common symptoms in kidney disease cats.
Is your pet’s name on the top 1200 list?
Get to the bottom of that bad breath!
Tips to keep your pet safe this holiday season
What is a diaphragmatic hernia?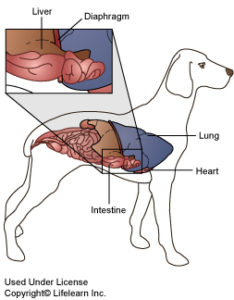 The diaphragm is the muscular partition that separates the abdomen and the chest. Tearing or disruption of this thin muscle is called a diaphragmatic hernia ordiaphragmatic rupture. The terms can be used synonymously. One form of diaphragmatic hernia, a peritoneal-pericardial diaphragmatic hernia (PPDH) is congenital, and is due to defective development of the diaphragm in the fetus. This condition is most often found in puppies or kittens and should be considered separately from the traumatic type of diaphragmatic hernia. Congenital diaphragmatic hernias are a recognized problem in Weimeraners and cocker spaniels.
The diaphragm is the muscular partition that separates the abdomen and the chest. Tearing or disruption of this thin muscle is called a diaphragmatic hernia ordiaphragmatic rupture. The terms can be used synonymously. One form of diaphragmatic hernia, a peritoneal-pericardial diaphragmatic hernia (PPDH) is congenital, and is due to defective development of the diaphragm in the fetus. This condition is most often found in puppies or kittens and should be considered separately from the traumatic type of diaphragmatic hernia. Congenital diaphragmatic hernias are a recognized problem in Weimeraners and cocker spaniels.
Once a tear in the diaphragm is present, abdominal contents such as the stomach, liver, and intestines are able to enter the chest cavity. This compresses the lungs and prevents them from fully inflating, causing respiratory distress. The abdominal tissues may irritate the heart muscle, which may cause abnormal heart rhythms. Fluid may leak into the chest cavity from the abdomen, further complicating and worsening heart and lung function.
What causes a diaphragmatic hernia or rupture?
“The most common cause of a diaphragmatic hernia is blunt force trauma.”
The most common cause of a diaphragmatic hernia is blunt force trauma. This type of trauma can occur after a fall from a high place (such as out of a window), an automobile accident or a blow to the abdomen. Congenital diaphragmatic hernias are less commonly seen.
What are the clinical signs of diaphragmatic hernia?
Clinical signs are dependent on the severity of herniation. With small tears or in dogs born with a diaphragmatic hernia, there may be no discernable clinical signs. The pet owner may report non-specific symptoms such as mild breathing difficulties, especially when stressed or exercising, and periods of mild gastrointestinal upset. In severe or acute cases, there is often respiratory distress, an abnormal heart rhythm, muffled heart and lung sounds and other signs of systemic shock. The abdomen may feel empty when palpated.
How is a diaphragmatic hernia diagnosed?
Diagnosis is based on medical history, physical examination findings and radiographs. Blood and urine tests may be performed if the patient is showing signs of shock. In certain cases, ultrasound or special radiographic dye studies will be required for a definitive diagnosis.
What is the treatment for diaphragmatic hernia? If there is a history of recent trauma, the dog must be stabilized before the hernia can be corrected. Some patients will require emergency thoracocentesis (a chest ‘tap’) to remove any fluid that has accumulated in the chest cavity.
If there is a history of recent trauma, the dog must be stabilized before the hernia can be corrected. Some patients will require emergency thoracocentesis (a chest ‘tap’) to remove any fluid that has accumulated in the chest cavity.
“Once the patient is stable, the hernia must be corrected surgically.”
Once the patient is stable, the hernia must be corrected surgically. In congenital forms, surgical intervention as early as possible is important to prevent organ entrapment or scarring between the abdomen and the chest. Many congenital diaphragmatic hernias are discovered during ovariohysterectomy surgery, and are corrected at that time.
What is the prognosis?
The prognosis for any patient with diaphragmatic hernia is always initially guarded. It improves once the patient has been stabilized and if the heart rhythm is normal. After surgery, a condition called re-expansion pulmonary edema may occur. Thus, a guarded prognosis must be given for at least twenty-fours after an apparently successful surgery. The prognosis for a young puppy with a congenital diaphragmatic hernia is guarded to good, depending on the specific diaphragmatic defect and the abnormalities found during surgical correction.
If the patient stabilizes with medical treatment, is it possible to avoid surgery?
In trauma cases, adhesions may form between the lungs and any herniated abdominal contents after approximately seven days.
“The longer the corrective surgery is delayed, the more complicated and dangerous it becomes.”
These adhesions will affect the ability of the lungs to inflate properly. The longer the corrective surgery is delayed, the more complicated and dangerous it becomes. However, each case needs to be assessed individually.
This client information sheet is based on material written by: Ernest Ward, DVM
What you need to know about Congestive Heart Failure.
Dog-gone good photo booth pictures
No turkey and trimmings for Fido
Heartworms aren’t just for the dogs
Anal Sac Disease in Dogs
What are the anal sacs?
anal_sac_disease_-_1_-_2009Commonly called ‘anal glands’, the anal sacs are two small pouches located on either side of the anus at approximately the four o’clock and eight o’clock positions. Numerous specialized sebaceous (sweat) glands that produce a foul smelling secretion line the walls of the sacs. Each sac is connected to the outside by a small duct that opens just inside the anus.
What is their function?
The secretion acts as a territorial marker – a dog’s ‘calling card’. The sacs are present in both male and female dogs and some of the secretion is squeezed out onto the feces by muscular contractions when the dog defecates. This is why dogs are so interested in smelling one another’s feces.
Why are the anal sacs causing a problem in my dog?
Anal sac disease is very common in dogs. The sacs frequently become impacted, usually due to inflammation of the ducts. The secretion within the impacted sacs will thicken and the sacs will become swollen and distended. It is then painful for your dog to pass feces. The secreted material within the anal sacs is an ideal medium for bacterial growth, allowing abscesses to form. The abscess will appear as a painful, red, hot swelling on one or both sides of the anus. If the abscess bursts, it will release a quantity of greenish yellow or bloody pus. If left untreated, the infection can quickly spread and cause severe damage to the anus and rectum.
How will I know if my dog has anal sac problems?
“The first sign is often scooting or dragging the rear along the ground.”
The first sign is often scooting or dragging the rear along the ground. There may be excessive licking or biting, often at the root of the tail rather than the anal area. Anal sac disease is very painful. Even normally gentle dogs may snap or growl if you touch the tail or anus when they have anal sac disease. If the anal sac ruptures, you may see blood or pus draining from the rectum.
In some cases, the dog had an episode of diarrhea or digestive upset a week or two before the clinical signs of anal sac disease became evident.
If your pet is showing signs of Anal Sac Disease do not wait as an impacted anal sac could lead to a rupture . Contact your local VCA Veterinarian. We offer a free first exam* for new clients.
How is anal sac disease treated?
Problems with the anal sacs are common in all dogs, regardless of size or breed. If you are concerned that your pet may have an anal sac problem, call your veterinarian at once. Treatment for impaction involves expressing or emptying the sacs. If the impaction is severe or if there is an infection, it may be necessary to flush out the affected sac to remove the solidified material. Since these conditions are painful, many pets will require a sedative or an anesthetic for this treatment. Antibiotics are often prescribed and sometimes may need to be instilled into the sacs over a period of several days. In advanced or severe cases, surgery may be necessary. Most dogs will require pain relief medications for several days until the swelling and inflammation have subsided.
Is the condition likely to recur?
Some dogs will have recurrent anal sac impactions or abscesses.
“Overweight dogs tend to have chronic anal sac problems because their anal sacs do not empty well.”
Overweight dogs tend to have chronic anal sac problems because their anal sacs do not empty well. Each impaction may cause further scarring and narrowing of the ducts, leading to recurrences that are even more frequent. If this condition recurs frequently, surgical removal of the sacs is indicated.
Are anal sacs necessary for my dog? Will removal have any adverse effects?
Anal glands produce the pungent smelling secretion that allows the dog to mark his or her territory. For our domesticated dogs, this is an unnecessary behavior and removal will not adversely affect your pet.
Are there any risks associated with surgical removal of the anal sacs?
“Removal of the anal sacs is a delicate and specialized surgery.”
Removal of the anal sacs is a delicate and specialized surgery. Some veterinarians perform this procedure routinely; however, in severe cases, your veterinarian may recommend referral to a board-certified veterinary surgeon. Some dogs will experience loose stools or lack of bowel control for one to three weeks following surgery. This occurs because the nerves controlling the anal sphincters (muscles that close the rectum) run through the soft tissues near the anal sacs. If the infection is deep and extensive it can be impossible to avoid damaging the nerves during the surgery. This damage resolves without further treatment in the majority of pets. In rare cases, the nerve damage is permanent, and e, it can result in fecal incontinence or the inability to control bowel movements, with constant leakage of feces from your dog’s anus.
As with any surgery, general anesthesia is required, this always carries some degree of risk. Advances in anesthesia drugs and monitoring continue to decrease these risks. For dogs suffering from chronic or recurrent anal sac infection or impaction, surgical removal is the best option to relieve the pet’s pain.
My dog is very nervous and sometimes seems to express his own glands. Is this normal?
“It is common for dogs to release the contents of their anal sacs, particularly if frightened.”
It is common for dogs to release the contents of their anal sacs, particularly if frightened. Some dogs even appear to lack control of the anus or anal sac ducts so that small quantities of fluid will drain out when they are resting, leaving an unpleasant lingering odor in the home. If your dog has this problem, you may elect to remove the anal sacs.
This client information sheet is based on material written by: Ernest Ward, DVM
Pet safety: winter plants to avoid
Do you and your dog like to hike? Check out the top 8 trails in the US.
Do you know what to do in a poisoning emergency?
Providing adequate housing for your guinea pig
It’s National Pet Diabetes Month -increase your awareness of this common disease
Feline asthma can be a complex disease
Planes, trains, automobiles, and your pet!
What to know about fall toxins
Helpful hints about aural hematomas
Does your dog show signs of stress? Here’s how to help!
Be helpful in a heat stroke situation.
7 surprisingly simple life hacks for you and your cat
Acetaminophen toxicity—what you need to know.
10 steps to keeping your cat’s teeth healthy.
What you need to know about TPLO surgery.
Pointers for walking your pooch.
Does your cat have patella problems?
Did you know total hip replacements are available for dogs?
10 Ways to Help an Arthritic Dog
August 24, 2011
When your dog is in pain, you want to help him feel better — fast. Luckily, there are quite a few things you can do to relieve the aches that are an everyday occurrence for dogs with arthritis:
- Take your dog in for regular checkups so that your veterinarian can monitor your pet’s arthritis and make necessary adjustments to the treatment plan.
- Getting or keeping your dog slim can help by decreasing the load on his joints. Your best bet: feeding your dog the right amount of high-quality food.
- Controlled exercise is a must, but make sure you carefully monitor your dog while she plays, walks, or runs. If possible, find a soft surface for activity. Your veterinarian can offer more suggestions for getting your dog moving regularly.
- As much as possible, keep your dog warm and dry, since cold and damp conditions can aggravate arthritis. Consider investing in a padded dog bed and apply warm compresses to painful joints.
- Ask your veterinarian for a recommendation to a professional animal massage therapist, as massage can increase your dog’s flexibility, circulation, and sense of well-being.
- Pain medication, including nonsteroidal anti-inflammatory drugs (commonly called NSAIDs), may help relieve pain, and disease-modifying osteoarthritis drugs (DMOADs) can also play an important role. Talk to your veterinarian before giving your dog any medication.
- Glucosamine and chondroitin supplements can be used to help improve joint mobility and support better joint functioning for dogs with arthritis.
- Acupuncture isn’t just for people. This painless technique has shown some success in animals suffering from arthritis.
- If your dog’s arthritis is advanced, surgery may be an option. Ask your veterinarian about the pros and cons of surgery and what you can expect.
- Be sure to take steps to adjust his environment at home. Some things that can help an arthritic dog include: providing soft supportive bedding for his achy joints, using ramps to help a dog get in and out of a car or up to a bed, and putting down carpeting and secure rugs to help him get traction as he walks.
Remember: A low-stress environment, plenty of affection, and supportive care can help your dog feel so much better.
This article has been reviewed by a Veterinarian.
Essential Tips for Every Cat Owner
Essential information on hip dysplasia
Thinking of getting a bird? Ask yourself these questions first!
Suggestions for keeping your indoor cat healthy and happy.
Dog Swimming Safety Tips
BY GINA SPADAFORI | JUNE 28, 2010
They didn’t coin the term “doggy paddle” because canines stay on shore. Many dogs enjoy swimming as much as people do, and cool times in the local swimming spot are irreplaceable summer experiences. But you have to look out for your pet around water, since even the strongest, most enthusiastic swimmers can get into trouble. The keys to water safety for dogs are prevention, preparedness and awareness.
Prevention
No dog should be given unsupervised access to a backyard pool, neighborhood pond or creek. Swimming pools are best fenced off for safety. If that’s not possible, they should be equipped with alarms that sound when the surface of the water is broken by a child or pet falling in and a ramp to help them find their way out.
Prevention also means teaching your pet what to do when he’s in the pool. Dogs don’t always understand that the steps are on a certain side, and they may tire while trying to crawl their way out. If your pet likes to swim, work with him in the pool to help him learn where the steps are so he can get out easily. Some breeds of dogs, such as bulldogs, pugs and basset hounds, do not have the body conformation to make them natural swimmers, and may need to be taught how to swim.
Obedience training is extremely important. Your dog should come when called, even when swimming. Emergency shortcut: Always carry extra retrieving toys. A dog who’s heading into a dangerous area after a ball or stick can often be lured back to shore with a second item. It’s no substitute for training, but it could save your dog’s life.
Preparedness
Before letting your dog swim in natural surroundings, survey the area for safety. Rivers and oceans can change frequently, and an area that was once safe for swimming can become treacherous. Consider currents, tides, underwater hazards and even the condition of the water. In the late summer, algae scum on the top of standing water can be toxic, producing substances that can kill a pet who swallows the water. When in doubt, treat it like you would a child: better safe than sorry.
One of the best things you can do is to take courses in pet first aid and CPR. Many local Red Cross chapters offer these classes, and some veterinarians in your community may teach them. A near-death dog rescued from the water may be saved by your prompt actions — if you know what to do.
If your dog isn’t much of a swimmer or is older or debilitated, get him a personal floatation device. These are especially great for family boating trips, because most have sturdy handles for rescue when a pet goes overboard.
Awareness
Be aware of your dog’s condition as he plays. Remember that even swimming dogs can get hot, so bring fresh water and offer it at every opportunity. When your dog is tiring, call it a day. A tired dog is a good dog, but an exhausted dog is in danger of drowning.
Be particularly careful with young and old dogs. Young dogs can panic in the water, and old dogs may not realize they aren’t as strong as they used to be. Keep them close to shore, and keep swimming sessions short.
Puppies can get acne just like humans.
Allergy Testing
FEBRUARY 21, 2014
Allergy testing is most commonly performed to determine if a pet has atopy, also known as atopic dermatitis or allergic inhalant dermatitis.
Allergy tests can help identify the specific allergens causing a pet’s allergy problem. Once a list of “problem” allergens is identified, a specialized serum containing small quantities of these allergens can be formulated specifically for your pet.
Allergy testing poses minimal risk for your pet, and in many cases the information your veterinarian gains from this testing is invaluable.
What Allergies Can Pets Have?
The most common types of allergies in pets are flea allergy, food allergy, and a condition called atopy. Atopy is sometimes called atopic dermatitis or allergic inhalant dermatitis, and it occurs when allergens that are inhaled or that contact the skin cause an allergic reaction in the body. In dogs (and, less commonly, cats), this allergic reaction is focused largely in the skin. Animals with atopy become very itchy; the resultant scratching can lead to skin injuries and subsequent skin infections. Atopy is usually first noticed in dogs younger than 3 years of age, although older pets can also be affected. Unfortunately, some pets that develop atopy continue to have problems throughout their lives.
Many types of allergens can cause a pet to develop atopy. A wide variety of pollens, grasses, dander, insect proteins (such as in cockroaches), molds, and even house dust can cause animals to develop atopy. Animals can even develop allergies to multiple allergens at the same time. Once an animal develops atopy, the condition will continue as long as the animal is exposed to the allergen that is the source of the problem.
How Is Allergy Testing Performed?
Allergy testing is most commonly performed to determine if a pet has atopy. Allergy testing can also help diagnose flea allergy dermatitis. Most veterinarians do not use allergy testing to diagnose food allergies.
The two most common types of allergy tests used in pets are intradermal skin testing and serum allergy testing:
Intradermal skin testing. Intradermal skin testing can sometimes be performed at your veterinarian’s office. However, because the allergens used for this test are very specific (they vary depending on where you live), your veterinarian may refer you to a veterinary dermatologist for this test to be performed. Usually, an area of fur is shaved from your pet’s side or abdomen to expose enough skin to perform the test. Using very small needles, tiny amounts of each test allergen are injected just under your pet’s skin in different areas. After a brief waiting period, the injection sites are examined to measure the degree of local allergic response, such as redness or a small hive. Allergens that your pet is not allergic to will not cause a reaction, while allergens that your pet is allergic to will cause a reaction that corresponds to the severity of the allergy. Pets are monitored carefully during the procedure in case a serious reaction occurs and treatment is required.
Serum allergy testing. Serum allergy testing is performed at a laboratory using a small blood sample taken from your pet. Your veterinarian does not need to shave your pet or have special allergens on hand to perform this test. As with intradermal skin testing, the results of serum allergy testing can reveal which allergens are not causing an allergic reaction in your pet, which ones are causing a mild reaction, and which ones are causing a more serious reaction.
Depending on which type of allergy test is performed, you may need to discontinue your pet’s allergy medications for a period of time before the test. Otherwise, the test results may be affected. Your veterinarian will tell you which medications can be used and which ones may need to be discontinued.
What Does Allergy Testing Tell Your Veterinarian?
Allergy tests can help identify the specific allergens that may be at the root of a pet’s atopic dermatitis. Once a list of “problem” allergens is identified, a specialized serum containing small quantities of these allergens can be formulated specifically for your pet. Through injection of small amounts of the allergy serum over time, many pets experience a reduced response to the allergens. This treatment, called immunotherapy, generally must be continued for several months to years to achieve results. With immunotherapy, the pet owner usually administers the allergy serum injections at home. If you are uncomfortable giving the injections, ask your veterinary care team if the injections can be given at your veterinarian’s office. The first injections are more diluted, containing only tiny amounts of the problem allergens; each subsequent injection solution contains a slightly higher concentration of the allergens. Your veterinarian will schedule the injections according to specific guidelines — more frequently in the beginning, and eventually tapering to one injection every few weeks. Many pets respond to this program. Others may not, especially if they have other underlying conditions.
Is Allergy Testing Safe?
Very few risks are associated with performing allergy testing. If serum allergy testing is performed, drawing blood takes only a few seconds, and your veterinary team will take precautions to ensure that your pet is not injured during this procedure. Once blood is obtained, all further processing is performed at the veterinarian’s office or at a diagnostic laboratory, so there is no risk of harm to your pet.
If intradermal skin testing is performed, there is a slight risk of an allergic reaction if your pet responds seriously to some of the allergens being tested. However, pets are monitored very closely during the testing procedure, and if a reaction occurs, medications can quickly be administered to treat the problem.
In general, allergy testing poses minimal risks for your pet, and in many cases, the information your veterinarian gains from this testing is very valuable.
cool-kid-william-yuth-fighting-pet-overpopulation
7-reasons-your-cat-keeps-meowing
Brushing, bathing, and nail trimming. How often do you groom your cat?
Did you know that leaving the TV on while you’re away can help reduce separation anxiety in your dog?
A yearly physical exam is an important part of your pet’s preventive care routine.
Learn how hot spots in dogs are diagnosed and treated, and how you can prevent them.
Follow these 12 rules to stay safe when running with your dog.
Watch out for these pet poisons this spring!
Some good information for our friends that have hamsters. Top 10 ways to keep your hamster healthy.
Are human pain relievers toxic to dogs and cats?
You know you take care of your dog, but did you know they keep you healthy, too?
According to Trupanion Pet Insurance, these are the 10 most frequently diagnosed problems in dogs.
In an emergency, these tips may save your pets life. However, it should not replace veterinary care.
Follow these steps to poison proof your bathroom.
Find out why cats are prone to UTIs and how they are treated.
Do cats get cavities? Get the answer to this and 9 other cat dental questions.
How do you know if your dog has had a stroke?
New Year’s don’ts for your pet.
The “terrible twos” exist even in the dog world. Find out how to get through the rough patch.
15 things you can do to exercise your dog and steps for ensuring safety.
Going away for the holidays? Learn 5 boarding options for your pet.
Learn 7 medical reasons that may cause your pet to gain weight.
A proper diet is an important part of rabbit care. Learn what you should be feeding your rabbit.
Follow these tips to keep your pet safe on Thanksgiving.
Do you have a destructive cat? If so, find out ways to distract him from this bad behavior.
Learn the top 10 human medications that are poisonous to pets.
Learn the facts about reverse sneezing.
Does your cat mark its territory? Learn tips to stop this bad behavior.
Get answers to AVMA’s top 9 senior pet care questions.
Is your furry friend on the list of best dogs for new owners? Find out!
We’ve mentioned the dangerous toxins of Halloween before. With tomorrow being Halloween we just wanted to provide everyone a reminder. Find out the most dangerous Halloween toxins.
Slimming down overweight cats.
Are you considering spaying or neutering your furry friend? Find out the benefits!
Learn how to diagnose, treat, and prevent acute pancreatitis.
Blood work can uncover medical problems that you may be aware of. It’s important to have blood work done yearly and catch any diseases early.
Halloween Can Be Spooky for Pets
Many people like to have fun during the Halloween festivities, but our pets can truly be frightened by all of the noises and costumes. Halloween is a holiday with many dangers for our dogs and cats.
Dressing up is fun for humans, but may not be fun for our pets. If your pet tolerates a costume, keep in mind your pet must be comfortable at all times. Avoid any costumes that use rubber bands or anything that might constrict circulation or breathing. Likewise, avoid costumes with toxic paints, dyes, or that are edible.
Costumes on people can be equally scary to pets. Masks, large hats, and other costume accessories can confuse pets and may even trigger territorial instincts. It is not unusual for pets to act protective and fearful of people in costumes, even if they are normally very social with that person. Remember, you are responsible for controlling your pet and insuring that he doesn’t bite any guests.
Constant visitors to the door along with spooky sights and sounds may cause pets to escape and become injured in a variety of ways. Consider letting your dog spend Halloween inside with special treats, safe and secure. Even in a fenced yard, Halloween is not a good night for a dog to be outside. This is doubly true for cats: they may try to bolt out the door and even if they are allowed outside, they are more at risk for being hit by cars due to the high traffic from trick or treaters. Black cats, especially, are at a higher risk from human cruelty on Halloween. Consider keeping your cats in an interior room where they are unable to bolt out the door.
Some Halloween decorations can be unsafe for your pets. Fake cobwebs or anything resembling string can be tempting to cats, leading to an intestinal obstruction. candles, even inside pumpkins, can be easily knocked over, burning your pet or even lighting them (it has happened before) or your house on fire!
Keep pets away from all Halloween candy. Most people know that chocolate can be toxic to pets, even in small amounts. However lollipop sticks and foil wrappers can cause blockages in the intestinal tract. Candy sweetened with xylitol can cause a life threatening drop in blood sugar if ingested by a pet. Some pets can get an upset stomach just from eating a piece of candy, since it isn’t part of their regular diet.
These simple responsible precautions will help humans and pets alike have a safe holiday. For more information on how to make Halloween less stressful to your pet, contact your veterinarian.
Created by M. Kathleen Shaw, DVM
National Preparedness Month
Did you know that September is National Preparedness Month? Since every community has different risks, it is important to know how to prepare for the risks associated with “your neck of the woods”. In Southern California, earthquakes pose the greatest risk and are the most likely natural disaster to affect our region. Many of us have an emergency plan for our family, but does this plan include your pet? Here are a few tips to prepare your pets should a natural disaster occur in your area.
One of the most important things to consider should a natural disaster hit suddenly and you become separated from your pets, is whether a stranger or animal control would be able to gather the necessary information to reunite you with your pet. Having your pet micro-chipped and current on all vaccines can facilitate a happy and rapid reunion in the event of a natural disaster. Proof of ownership is also an important component for a trouble free reunion. Any adoption or registration papers, micro-chip paperwork, medical/vaccine records, and a recent photo should be included in an emergency pet-care kit.
What else belongs in the emergency pet-care kit? Your emergency pet care kit should include the following:
- A seven day supply of food, water, and treats for each pet
- Portable feeding dishes
- All necessary medications
- Extra leashes
- Portable litter box for our feline pets
- Blankets or bedding
Finally, include your pet in the evacuation plan. It may be difficult in the chaos of a disaster to locate a pet, but having a plan in place can increase the odds of a successful evacuation. If a disaster should occur while you are away from home, having stickers at the front and back doors with the number of pets in the household and the name and phone number of your veterinarian will alert neighbors and emergency personnel and aid in the evacuation of your pets should you not be at home.
If any of your pets are not currently micro-chipped or current on vaccines please schedule an appointment today so we can help you properly prepare your pets in the event of a natural disaster.
Xylitol Toxicosis
What is Xylitol?
Xylitol is a white, crystalline sugar alcohol that is used as a sugar substitute sweetener in many products. It is found in sugar-free gum, candy and foods. It is also available in the granulated form for baking and is popular among diabetics and those on low-carbohydrate diets.
How is xylotol different in humas than dogs?
In humans, xylitol is absorbed slowly and has little to no effect on blood sugar or insulin levels. In dogs, Xylitol is quickly absorbed into the bloodstream and can cause profound hypoglycemia (low blood sugar). In dogs, Xylitol can also cause liver failure, bleeding and death. Xylitol’s effect on cats is not clear at this time.
How much Xylitol is toxic to my pet?
In general, we estimate that one to two pieces of gum could cause hypoglycemia in a 20 pound dog.
What are the symptoms?
Vomiting is often the first symptom. Signs of hypoglycemia also occur rapidly (lethargy, weakness). Diarrhea, collapse and seizures may also be seen.
Is Xylitol poisoning treatable?
All Xylitol exposure should be evaluated by a veterinarian immediately. This is important because of the rapid absorption of Xylitol. There is no antidote for Xylitol toxicity. Remember that even a tiny dose can be toxic to dogs. Treatment would consist of supportive care and close monitoring of blood glucose levels.
How can we avoid Xylitol toxicosis?
Keep all sweets, gum and foods that contain Xylitol out of reach of all pets. Again, if an accidental exposure is suspected, seek veterinary care immediately! It is important to realize that products safe for humans are not always safe for our pets.
Dr. Voltin
The Poisons of Summer
June, July and August are the most dangerous months of the year for companion animals, according to the Animal Poison Control Center. Last year, the center received the highest number of phone calls in July. Forty-three percent of those calls involved animals’ exposure to insecticides, rodenticides and herbicides.
We have compiled a list of lesser known toxins. As always, if you suspect that your pet has been exposed to or has ingested a potential toxin, please call our office immediately for recommendations on how to proceed.
* Charcoal Lighter Fluid
Contact with this toxic substance can cause an animals skin to dry and crack. Ingestion and inhalation can result in vomiting and rapid spread to the lungs. Ultimately, chemical lung infections can result.
* Grapes and Raisins
Kidney failure is possible after ingestion of any variety of grapes or raisins.
* Macadamia Nuts
Dogs that eat large amounts of these nuts can suffer from transient hind limb paralysis (inability to use rear legs).
* Onions and Garlic
The disulfides in these plants cause a serious, life-threatening anemia. Beware of onion powder used in many baby foods.
* Hops Plugs
Pets that chew on hops plugs thrown away after brewing beer can develop hyperthermia (high temperature). Body temperature increases rapidly and can reach 103 to 105 degrees within hours.
* Glow-in-the-dark objects
Sold at fairs, carnivals and novelty stores, these objects contain the liquid dibutyl phthalate. Cats that ingest the liquid will drool and slobber excessively. The problem can resolve quickly (within minutes) but is usually quite distressing to pets and owners alike.
**As always, never leave your pets in a car or other confined area without adequate ventilation. Even with the windows cracked the temperature in a car during the summer can reach temperatures within minutes that can be fatal to animals.
We hope this information is helpful and that you all have a safe and happy summer!!
Dr. Voltin